1. Introduction
Code blue (CB) is used to indicate a patient who requires resuscitation, most often due to cardiopulmonary arrest (CPA) [1]. Hospitals have code blue teams to reduce preventable in-hospital deaths in Turkey. CB was introduced in practice in our country since 2009 [2].
Our hospital has a CB team composed of an anaesthesiologist, an anaesthesia technician educated in cardiopulmonary resuscitation (CPR), and a security guard to respond to all calls in all hospital areas except intensive care units (ICU) and the emergency room. The CB forms which are completed by anaesthesiologist as code blue team leader.
The primary object of the study is to evaluate the demographic data of the patients, and the outcomes of CB calls. In addition, we aimed to determine the rates of false CB calls and the clinics giving CB calls in our hospital.
2. Material and Methods
2.1 Ethics statement
After approval was obtained from the ethics committee and hospital administration (Karabuk Universty Ethics Committee, no: 6/16, date: 30/05/2018), this study was conducted at the Karabuk University Hospital, a new tertiary academic hospital in Karabuk, Turkey that has 400 beds. Informed consent forms were obtained from each patients or their legal representatives. The study was carried out in accordance with the Declaration of Helsinki.
2.2 Study criteria
The CB forms used between January 2017 and January 2018 in our hospital were retrospectively analyzed.
Variables such as; age, and gender of the patients, the time of the calls, the arrival time of the team, which parts of hospital activated the CB, the rates of false CB calls, the results of patient’s last status (classified as exitus, transferred to ICU, and continued care in ward) were recorded. Files with missing data were excluded.
The calls occurrence time was grouped as work hours (weekdays between 08:00–16:00), and shift hours (weekdays between 16:00- 08:00, and weekend). Official holidays and festivals were included in the shift hours.
Arrival time of the team was regarded as the time between CB call and the arrival of the team.
In-hospital cardiac arrest according to Utstein model; a patient who does not need basic life support or advanced life support is defined as a false arrest.
2.3 Data analysis
Data were analysed using SPSS 16.0 for Windows (SPSS). Descriptive statistics of the demographic data and constant variables were indicated as mean ± standard deviation. Statistical significance of the differences among the mean values was calculated using Student’s t-tests. Fisher’s exact tests or chi-square tests were used to analyse the incidence data. Data with a p value under .05 (p < .05) was accepted as statistically significant.
3. Results
We had 230 CB calls in the study period. Five of them were excluded because of incomplete data. The mean age of the patients was found to be 75.14 ± 12.86. In this series, 126 (56%) men, and 99 (44%) were women. The mean arrival time of the team was 1.97±0.72 minutes (min).
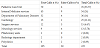
The most code in our hospital is given in Palliative Care Unit (76 patients, 33.77 %) followed by Internal Medicine Services (54 patients, 24%), and Department of Pulmonary Diseases (36 patients, 16%).The number of false CB announcements was found to be 30 (13.33%). The CB calls numbers and false calls numbers of services are summarized in the Table 1 (The code blue calls numbers and false calls numbers of services).
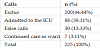
The evaluation of the outcomes of CB calls showed that 100 patients were exit us; and 88 patients had been admitted to the ICU; 7 had been continued care in ward by a successful intervention Table 2.
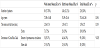
Most of the CB calls (140 calls, 62.22%) were during off times. The comparison of work hours and shift hours blue code calls is summarized in Table 3.
4. Discussion
In our study, the mean arrival time of the team was 1.97±0.72 min, which was in accordance with the Ministry of Health's quality standards. We found that the Palliative Care Unit gave the most CB. Most of the CB calls (140 calls, 62.22%) were during off times. Thirty of the 225 CB call were false. Of the remaining 195 patients, 100 died and 88 patients received ICU.
Cardio pulmonary arrest (CPA) is sudden cessation of breathing or circulation [3]. The CB team should arrive to the call location within 3 min to start CPR. This is very vital for the patient with arrest, because delayed intervention increases mortality and worsens neurological sequelae [4].
Ristagno et al. found that starting CPR in 1.5-3 min was more successful than starting the procedure more than 5 min after the CPA [5]. In studies, arrival times varied between 1.3 min and 5.7 min [6,7] .
In several studies performed in Turkey, different arrival times have been reported. Eroglu et al. reported this time as 105 seconds [8]. The arrival time was 2.17 min in a study by Bal et al. [9], Bayramoglu et al. found this time as 4.31 min [10]. In the present study, the mean arrival time was 1.97±0.72 min. which is consistent with the literature.
According to the locations of the CB calls, most of the calls were made from the Palliative Care Unit, followed by Internal Medicine services and Department of Pulmonary Diseases. Bayramoglu et al. reported that most of CB calls were given by services [10]. In our hospital; CB calls are not applied in ICU and emergency units. This may be caused by the monitoring of patients with critical disease in services.
The time of the CB calls during work hours and shift hours has been investigated in several studies. Pattnaik et al. found that most of the CB calls (72.46%) were during off times [11]. Cicekci et al. stated that 32.6% of the CB calls were in working hours [12]. Bakan et al. reported that true CB calls were given often out of working hours (66.82%) [13]. In our study, we found this rate as 62.22 %.
Kaykısız et al. reported that the rate of false CB calls was 45% [14]. In a study performed by Kaernested et al, 231 of 311 patients’ CB calls were false [15]. Canural et al. found the false code rate as 61% [16]. In our study, the rate of false calls was 13.33%. We believe that this rate does not reflect reality, because most of the false code calls are not recorded in our hospital.
Bal et al. reported that 90 of 137 patients survived [9]. Pembeci et al. found that the survival rate was 49% [17]. Bakan et al. reported this rate as 37.92% [13].
5. Conclusion
In our study, we found that 44.44 % of patients had been exitus; 39.11 % of patients had been admitted to ICU; and 3.11 % of patients had been continued care in ward. The number of deaths in ICU could not be assessed due to retrospective nature of the study.
This study is a single-center, and nonrandomized study. The longterm mortality of living patients could not be assessed due to the retrospective nature of the study. The comorbidities, hospitalization diagnoses, and vital signs of the patients could not be determined as a result of missing records. The CB form mostly was not recorded for false CB calls. As a result of this, we think that the false CB rate was higher.
The CB calls were more common during off-hours and the absence of night duty doctor at the services especially in rural hospitals like ours; demonstrate the importance of maintaining this system uninterruptedly. In this study, we noticed that we should be more attentive in recording code blue forms to assess precisely the effectiveness of the system. It is also necessary to identify and eliminate deficiencies in the code blue system.
Competing Interests
The authors declare that they have no competing interests.