1. Introduction
Nanosecond pulse electric field refers to a kind of pulse electric field whose pulse width is at the nanosecond level, this kind of electric field can produce reversible electroporation [1] and irreversible electroporation (IRE) [2] on the cell membrane. Reversible electroporation is a transient hydrophilic hole in the cell membrane induced by the pulsed electric field [3]. This phenomenon was first discovered by Neumann and Rosenheck that electrical impulses caused changes in the permeability of the membrane [4]. Then Zim-mermann et al. found that 1-10 kv/m pulse electric field can break through the red cell membrane, form a dielectric breakdown of the cell membrane, releasing hemoglobin, and the hemolytic mechanism causes cellular mechanical rupture or thermal rupture. At 37 °C ruptured cells closed again [5]. This phenomenon is called electroporation of the cell membrane.
However, Sale et al. found that under high voltage pulsed electric field, red blood cells and protoplast produce lysis and cell death [6]. Sun caixin et al. believed that with the increase of the pulsed electric field dose, the irreversible rupture of cell membrane caused cell death, which was called irreversible electric breakdown. It was observed that SKOV3 cells of human ovarian adenocarcinoma presented retained shape and complete cell membrane, but the mitochondrial swelling and cavitation showed the phenomenon of cell death caused by highvoltage pulsed electric field [7].
Since the FDA approved the Nanoknife in 2011, the IRE clinical application of nanosecond pulsed electric field showed an explosive growth. At the cell level, the biophysical mechanism of non-thermal irreversible electroporation of pulsed electric field was studied. At the animal level, we studied the 1 safety of irreversible electroporation and preclinical animal experiments, also the clinical application of irreversible electroporation.
2. Animal Studies of Irreversible Electroporation
Before the application of irreversible electroporation in clinic, the basis of animal experiment should be provided. These experiments can prove the beneficial effects and safety of IRE in tumor treatment and verify the potential of IRE in clinical treatment to some extent. This article summarize part of them.
2.1 The rabbit
In the experiment that irreversible electroporation could eradicate VX2 hepatic tumors in rabbits, IRE electrodes advanced toward the implanted tumor center from the three overlapping directions of lower, middle and lateral, covering all the implanted VX2 tumors to treat the entire tumor [8].
2.2 The canine
The first case of irreversible electroporation for intracranial canine proved that it is safe to use irreversible electroporation in canine intracranial surgery [9]. The safety of NTIRE in the brain was examined with specially designed dogs, and NTIRE was applied to the first step of local ablation treatment for brain cancer and other intracranial diseases [10]. Garcia et al. proved that the treatment of Malignant Glioma com-bined with NTIRE is rapid and minimally invasive, and effective in ablating pathologic heterogeneity brain tumor tissue without aggravating cerebral hemorrhage [11].
2.3 The swine
IRE treatment of pig pancreatic tissue is safe and effective. TTC staining predicted the resection of the pancreas within 2 hours after treatment. Further studies are needed to determine the optimal electrode spacing and voltage for IRE ablation in the pancreas. Further studies are needed to determine the role of IRE in pancreatic tumor ablation [12].
In the treatment of complete thickness ablation of normal pig bile duct, it is proved to be feasible and safe. Moreover, the thermal mechanism of RFA and laser ablation may cause the risk of deep tissue infiltration and perforation and cholangitis. IRE, by contrast, helps to insulate the extracellular matrix from the effects of ablation, reducing the risk of biliary penetration ablation, and reducing the incidence of adverse events [13].
The ablation of the colon [14], lymphaden [15], pancreatic tissue [16-18], gastric wall [19], epidural space of spine [20], liver [21], ureter [22], vertebrae [23] of the pig demonstrate the feasibility and security of IRE.
2.4 The rat
Guo et al. demonstrated the efficacy of IRE in targeted treatment of liver tumors in a transplanted mouse liver cancer model for the first time [24]. In the mouse experiments, IRE as a treatment for nonmetastatic pancreatic tumors showed significant anti-tumor effects and prolonged survival in mice [25]. It was found that irreversible electroporation could prolong the overall survival time of liver tumor mice and reduce the growth rate of tumor [26]. Synergistic effects between Moderate Heating and IRE have been demonstrated in in vitro tumor ablation and in vivo tumor reduction. Controllable and moderate heating can improve the efficacy of irreversible electroporation in the treatment of pancreatic cancer, and significantly expand the ablation area of tumor in vitro and reduce tumor growth in vivo [27].
3. Clinical Application of Irreversible Electroporation
Human clinical studies have begun after encouraging results in animal models.
3.1 Pancreatic cancer
Pancreatic cancer is one of the world's deadliest cancers, with a fiveyear survival rate as low as 6 percent. Most pancreatic cancer patients develop locally advanced or metastatic disease at diagnosis [28].
IRE ablation for locally advanced pancreatic cancer is safe and feasible and can be used as a major local treatment [29]. This metaanalysis suggested that IRE use may be safe and effective for prolonged survival in pancreatic cancer patients [30]. In the experiments conducted by Martin et al., 200 patients were followed at a median of 29 months, and the overall survival rate was observed at 19.25 months from the time of treatment [31].
Patients who had concurrent IRE therapy had greater local remission and improved overall survival compared to those who had only radiation and chemotherapy [32]. The recurrence rate was lower (3%) after a median follow-up of 29 months, suggesting that even in advanced patients, treatment with IRE after chemotherapy can inhibit tumor regeneration and significantly improve the quality of life [33]. Irreversible electroporation combined with allogeneic natural killer cell immunotherapy can significantly improve the median PFS and OS in stage iii pancreatic cancer and extend the median OS in stage IV pancreatic cancer. Multi-allogeneic natural killer cell infusion is associated with better prognosis of stage III pancreatic cancer [34].
Ansari et al. summarized a total of 446 patients in 10 studies. Percutaneous drainage was performed in 142 patients and in 304 patients [35]. Tumor size are between 2.8 and 4.5 centimeters. Postoperative complications occurred in 35% of patients, most of them less severe. Nine patients (2.0%) died after surgery. The technical success rate is 85-100%. The mean survival time of free recurrence after treatment of IRE was 2.7 to 12.4 months. The median postoperative overall survival was 7-23 months. Total survival was highest when IRE was combined with pancreatectomy.
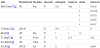
The information of IRE therapy to pancreatic cancer is listed in Table 1.
3.2 Liver cancer
Irreversible electroporation (IRE) is a new type of percutaneous ablation technology developed in the last decade, whose application in the treatment of primary and metastatic liver diseases is progressing rapidly [47].
Hepatocellular carcinoma (HCC) remains a major health concern at present because of its increasing incidence and the complexity of its treatment [48]. It has risen to become the third leading cause of cancer related deaths in the world, killing more than 800,000 people a year [49]. Studies have shown that IRE therapy for non-resected liver cancer is a viable, safe and effective treatment, and will not cause serious complications even if the excised lesions are close to the main branches of the portal vein. The diagnostic accuracy of MRI, CT, and CEUS for IRE treatment in HCC patients was similar during the 1, 3, and 6 months of follow-up to assess the ablative region [50].
The use of IRE should be included in a multidisciplinary discussion of the treatment of primary and secondary hepatic metastases around blood vessels. In addition, IRE therapy can give unresectable patients the opportunity to have a resection or a two-stage hepatectomy [51].
Kingham et al. investigated the safety of IRE in the treatment of hepatic malignant tumors by hepatic veins and portal veins [52]. CHEUNG et al. determined the therapeutic safety of liver malignancies near the central site of the main biliary tract [53]. An irreversible electrical perforation (IRE) was successfully treated for a 65-year-old man with hepatocellular carcinoma [54]. The safety of IRE indicates that the integrity of the central structures such as the bile duct, hepatic artery, and portal vein can be protected after the IRE treatment [55].
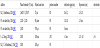
The information of IRE therapy to liver cancer is listed in Table 2.
3.3 Prostatic cancer
Irreversible electroporation has been used in clinical practice for many years as a non-thermal therapy for prostate cancer [61]. Data support IRE as a viable treatment for all prostate segments, with no significant differences in quality of life effects [62]. Irreversible electroporation is effective for the ablation of prostate tumors, since most men do not find any signs of residual cancer when they are biopsied six months after the ablation [63]. Irreversible electroporation ablation is mainly manifested as fibrosis, necrosis and epithelial detachment of glandular structure. The ablation zone is well demarcated, showing a clear line between viable and non-viable tissue [64].
Formally, there is no fundamental difference between IRE's risk and the procedures established to date to treat localized prostate cancer [65]. Irreversible electroporation (IRE) treatment for local prostate cancer (PCA) is still considered experimental, although initial results confirm its high developmental potential as a local treatment for organ and functional protection [66]. Van den Bos et al. described ablation sites as two to three times larger than expected and spread from the prostate capsule to the neurovascular bundle, which carries the associated risk of stress incontinence and erectile dysfunction [67].
The information of IRE therapy to prostatic can-cer is listed in Table 3.
3.4 Breast cancer
Currently, the clinical treatment of breast cancer usually includes the combined treatment of surgical excision or mastectomy, radiotherapy and adjuvant chemotherapy [71]. One study suggested that IRE could be a favorable option for surgical resection of the breast reserved treatment [72]. Rapid lesion clearance will allow healthy cells to repopulate the initially affected areas and treatment margin [73].
The electric field applied to the thymic matrix lymphopoietin (TSLP) signal can be affected when IRE uses short-time transient voltage, and the molecule has known pro-tumor effects through immune-cell phenotype regulation [74].
4. Irreversible Electroporation and Imaging
Similar to radiotherapy treatment, traditional medical imaging methods such as CT, magnetic resonance imaging (MRI) and ultrasound imaging can be used in preoperative and intraoperative treatment plans to determine effective tissue volume ablation [74].
Different organizations should apply different imaging methods according to the actual situation. Such as: The anatomical structure of hepatic portal is complex, and the distance between hepatic duct, portal vein and hepatic artery is close. Hemorrhagic fever with renal syndrome may be associated with serious complications. In one study, percutaneous electrode placement will be guided by CT fluoroscopy through catheter arteriography to prevent major vascular puncture or electrode placement too close to an important structure [56].
The position of the electrode can be shown on the ultrasound image. The distance between a single pair of electrodes was measure. Based on these measurements, the software installed on the IRE device can calculate the voltage required to produce the ablative electric field. The changes of perfusion in the ablation zone after IRE injection were observed by contrast-enhanced ultrasonography. The technique allows for the localization of electrodes around all patients under image guidance. Target lesions and safe boundaries were within the estimated range of ablation. MRI-TRUS guidance combines the advantages of good visualization of the target lesions by MRI with ultrasound's ability to obtain imaging in real time via mobile devices [75].
5. Future and Challenges
In one study of IRE ablation, all tumors were smaller than 3.5 centimeters, except for one tumor whose maximum diameter was greater than 3.5 centimeters [76]. However, if the tumors with a diameter of 3-4cm are ablated by IRE, the complete ablation rate will be reduced and the possibility of recurrence will be increased [77].
Numerical and experimental results show that the heterogeneity of liver tissue affects the uniformity of the distribution in the midfield during the treatment of IRE, leading to uneven cell death [78]. The electric field intensity increased in the area around the vessels in the plane perpendicular to the electrode, but decreased significantly in the tissue around the vessels in the parallel plane.
The use of IRE in the liver is limited in tumors which are larger than 3 cm and limited in operative time. These two factors, along with cost, have prevented IRE from becoming the only certain pattern for all liver tumor ablation. As this technique continues to develop, IRE therapy will increasingly become an ablative treatment for most liver cancers [47].
IRE is not only a promising surgical tissue ablation technique, but also a gene therapy technique. Since IRE ablation may leave intact tumor antigens, these findings have promoted clinical studies of tumor ablation, using immune-stimulating plasmids for the combination of local eradication and systemic immunotherapy [79]. The application of IRE-isogene NK immunotherapy is a new and promising combination therapy [80]. However, larger clinical trials are still needed to confirm these conclusions.
IRE will cause muscle contractions, and H-FIRE seems to be an effective technique to mitigate muscle contractions associated with traditional IRE pulses [81].
Given that the rate of progress has become a viable ablative technique for treating liver malignancies, electroporation may be the preferred ablative treatment for most patients over the next five years. As people's understanding of potential applications from IRE gets wider and wider, and technological advances become more widespread, applications become more common.
Competing Interests
The authors declare that they have no competing interests.