1. Introduction
Heparin-induced thrombocytopenia (HIT) is an adverse drug reaction mediated by platelet-activating antibodies that target complexes of platelet factor 4 and heparin, which is a potentially fatal clinical disease usually due to the administration of various forms of heparin (e.g. unfractionated or low-molecular-weight heparins). Even small doses of heparin such as heparin flushes in hemodialysis catheter can also induce the development of HIT [1,2]. Up to 8% of patients receiving heparin are at risk to develop HIT antibodies, but only 1-5% on heparin will progress to develop HIT with thrombocytopenia and subsequently one third of them may suffer from arterial and/or venous thrombosis [3]. HIT is caused by the formation of abnormal antibodies that activate platelets. The treatment of HIT requires stopping heparin, and both protection from thrombosis and choice of an agent that will not reduce the platelet count any further. Several alternatives are available for this purpose and mainly used are fondaparinux, danaparoid, argatroban and bivalirudin [4]. Here, we present the case of a 37-year-old hemodialysis patient with end stage renal disease and acute heart failure, who was diagnosed as HIT and received anticoagulation with citrate dialysis and argatroban to prevent thrombosis.
2. Case Report
A 37-year-old male patient with end stage renal disease was admitted to our hospital for evaluation of chest tightness, difficulty of lying down and increased serum creatinine. His blood pressure was 177/100 mmHg, and body weight was 99.5 kg. There were some small rough breathing sounds. Computed tomography of chest revealed increased bronchovascular markings in both lung fields and thin pericardial effusions. Laboratory findings included: blood pH 7.31, partial pressure of oxygen 8.62 kPa, standard bicarbonate 16.9 mmol/L, potassium 5.7 mmol/L, hemoglobin 88 g/L, albumin 45 g/L and NT-pro BNP 21860 pg/mL. The patient’s renal function was severely impaired: serum creatinine was 1057 μmol/L and GFR (calculated using CKD-EPI equation) was 4.8 mL/min. Ultrasound demonstrated shrinking kidneys (right kidney 91*43 mm, left kidney 86*37 mm). On the first hospital day, a hemodialysis catheter was inserted at his femoral vein and continuous renal replacement therapy (CRRT) was initiated with regular doses (18-22 mg/h) of heparin to prevent thrombosis of extracorporeal circuits. The patient received four sessions of CRRT and one session of hemodialysis. The patient’s platelet count markedly decreased from 118×109/L to 42×109/L on the ninth day after his first heparin administration, and no other explanations of thrombocytopenia were found.
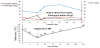
The patient’s 4Ts score was 6 points (high probability of developing HIT) based on the >50% platelet count fall (2 points) after nine days of LMWH exposure (2 points) plus the absence of other plausible causes of thrombocytopenia (2 points). The heparin-platelet factor 4 antibody by enzyme-linked immunosorbent assay (ELISA) was positive (6.9 U/ mL). Based on the probability of HIT and laboratory confirmation, we diagnosed the patient as having HIT and discontinued the use of heparin. Dialysis regimen was changed to citrate, and argatroban was administered at 0.5 mcg/kg/min on account of his edema and heart failure situation. Argatroban treatment was monitored daily with the activated partial thromboplastin time (APPT) with target 1.5-3.0 baseline. The patient’s thrombocytopenia started to resolve, and a platelet count of 101×109/L was reached on the twenty-first hospital day (twelve days after heparin suspension). His time course of platelet count changes was illustrated in Figure 1. There was no thromboembolic complication. The patient was well and stable, and was discharged with a platelet count of 143×109/L.
3. Discussion
HIT is an immune-mediated adverse drug effect in which significant drop in platelet count is the most common manifestation that typically occurs after 5-14 days of exposure to unfractionated heparin (UFH) or lower-molecular-weight heparin (LMWH), creating a considerably increased risk of venous and arterial thromboses [5-7]. The percentage of platelet drop can be up to 30% or greater than 50% of the baseline value. HIT is associated with significant morbidity and mortality if unrecognized [8,9]. Due to continuous exposure to heparin, dialysis patients are a risk group and up to 12% of them develop HIT [10].
Diagnosis of HIT is a combination of clinical presentation and laboratory findings. The 4Ts scoring system assesses the readily available clinical features, and is used for estimating the likelihood of HIT in thrombocytopenia patients treated with heparin while waiting for laboratory results for antibodies. A score of 0-3 indicates a low probability of HIT, score of 4-5 indicates intermediate probability, and score of 6-8 indicates high probability. If the 4Ts score represents intermedia or high probability, a presumptive diagnosis of HIT should be made, and laboratory testing should be requested [11]. Two types of assays are available, which include a functional (platelet activation) assay and antigenic assay (ELISA). In the patient case, his 4Ts score was 6 points. Although we did not have access to a functional assay, the patient did test positive for heparin-platelet factor 4 antibodies by ELISA, and we therefore diagnosed the patient as HIT.
The cornerstone of HIT management is the immediate discontinuation of all forms of heparin (UFH or LMWH) and administration of a non-heparin anticoagulant. Heparin locking solution in the hemodialysis catheters and heparin rinsing of the hemodialysis circuit have also been reported to be the cause of HIT. Therefore, it should be removed or replaced with unheparinized saline. Argatroban, danaparoid, fondaparinux and bivalirudin are available as non-heparin anticoagulants for HIT patients. Choice of a nonheparin anticoagulant should be based on the patient’s liver and renal function, clinical condition and drug availability. Argatroban and bivalirudin are preferred agents for impaired kidney function patients, as well as for patients with combined hepatic and renal failure [10,13]. Argatroban is administered via continuous intravenous infusion at a dose of 2 mcg/kg/min, and dose is adjusted to 0.5 mcg/kg/min in case of liver dysfunction [13,14]. For dialysis patients, other therapeutic methods can also be implemented such as citrate dialysis, peritoneal dialysis and plasmapheresis [15,16]. As recommended, we promptly stopped the use of heparin and changed to citrate dialysis along with the administration of an alternative non-heparin anticoagulant, argatroban. The treatment period was successful with gradual platelet count recovery between day 9 and 33, with no thrombosis or other complications noted. The discontinuation of heparin regimen and the subsequent use of citrate and argatroban were safe and effective. However, argatroban has not been approved for the HIT treatment in China.
Some studies have proved novel oral anticoagulants (NOACs) such as rivaroxaban, dabigatran, and apixaban to be safe and effective as alternative agents in the treatment of HIT [17-19]. NOACs do not require routine laboratory monitoring, and have a lower risk of bleeding, but further data is warranted for definite approval. For dialysis patients with a history of HIT, re-exposure to heparin should be avoided, and use of argatroban, danaparoid beside dialysis circuit flush with saline and citrate should be considered [20].
In conclusion, physicians must consider HIT in a dialysis patient who presents thrombocytopenia within 5-14 days after heparin exposure. In this case, we successfully treated a hemodialysis-related HIT patient with citrate dialysis and adjusted dose of argatroban. Since complications of HIT could be life-threatening, we emphasize the use of 4Ts scoring system in combination of laboratory assays for an early and accurate diagnosis of HIT. When HIT is suspected, all forms of heparin must be withdrawn in a timely manner, and alternative anticoagulation therapy should be initiated to prevent thrombotic events.
Competing Interests
The authors declare that they have no competing interests.
Author Contributions
Ming-ming Yan and Guo Ma: Participated in research design and
report analysis.
Shu-Shan Wu, Xiao-yan Qiu, Yu-ping Liu and Ye Liu: Participated in
the literature retrieval.
Ming-ming Yan, Shu-Shan Wu and Guo Ma: Wrote or contributed to
writing the manuscript.