1. Introduction
Escherichia coli is the most important clinical pathogen of hospital infection, and its broad-spectrum β-lactam resistance is of global concern. Broad-spectrum β-lactam resistance is commonly expressed by production of β-lactamases. Certain genes encoding β-lactamases are located on the plasmids; thereby, considered to spread over many species and strains [1]. In particular, in order to prevent selection of carbapenem resistant Enterobacteriaceae, which is one of serious problem in the world, it should be necessary to keep up surveillance and control of extended spectrum β-lactamase (ESBL) producing gram negative organisms [2].
Currently, CTX-M-15 type ESBL producing E. coli has notably been disseminated all over the world. Moreover, CTX-M-16, -27, and -55 type ESBL producing E. coli that possesses D240G amino acid substitution and confers ceftazidime resistance was also found [3,4]. In comparison with CTX-M-15 enzyme, CTX-M-55 enzyme is substituted by a single amino acid in mutated sites, A77V, and is classified as CTX-M-1 groups [5]. Since CTX-M-55 producing Enterobacteriaceae is often isolated from livestock and retail meat, moreover, it is suspected that ESBL producing bacteria spread to human through meat ingestion. Indeed, several reports support the suspicion that ESBL producing bacteria spread through the meat ingestion [6], having been prevailing in clinical patients and healthy humans [7].
However, characteristics of CTX-M-55 producing E. coli strains isolated from clinical patients are still unclear. The aim of the present study is to investigate molecular epidemiology and characteristics of CTX-M-55 producing E. coli isolated from medical facilities with less than 300 beds in Japan using next-generation sequencing.
2. Materials and Methods
2.1 Bacteria collection
Sixty-four isolates including CTX-M-1 group ESBL genes, which were selected from 207 ESBL positive E. coli isolated from medical facilities with less than 300 beds from February to October in 2016 in Kanagawa prefecture, Japan, were used as samples [8]. Classification of CTX-M groups was performed by multiplex PCR according to the study of Woodford et al [9]. Indeed, these isolates were characterized in commercial laboratories. Only one isolate per patient per facility was collected. However, the strain isolated from the same patient in different facilities was probably included. The isolates were collected with their information regarding specimen, clinical department, and patient status (inpatient or outpatient), as well as with facility information about number of beds and location.
2.2 Antimicrobial susceptibility testing
MICs were determined by the CLSI microdilution broth method [10]. Commercial microdilution broth plates “Neg EN MIC 1J” for antibiotic susceptibility testing were purchased from the Beckman Coulter.
2.3 Determination of blaCTX-M gene typing
The isolates were cultured for enrichment in LB broth (Nacalai Tesque) including 2mg/L cefotaxime (sigma), and whole DNAs were extracted by DNeasy Blood & Tissue Kit (QIAGEN). The blaCTX-M gene typing in CTX-M-1 group ESBL genes positive isolates was determined by direct sequencing. Primers for PCR were used as primers for direct sequencing [8,9].
2.4 Next-generation sequencing and data analysis
The isolates involving blaCTX-M-55 gene were cultured for enrichment in LB broth including 2mg/L cefotaxime, and whole DNAs of the strains were extracted by PureLink Genome DNA Kit (Thermo). The fragment library was constructed by Ion Xpress Plus Fragment Library Kit (Thermo). The DNA fragment was ligated to barcode and P1 adapters, and the 480 bp library fragment was collected by size selection. Ion Chef and Ion S5 system (Thermo) and Ion 530 Chip (Thermo) was employed for next-generation sequencing. Highthroughput sequencing data was analyzed for de novo assembly using Center for Genome Epidemiology (CGE) site [11]. Assembled contigs of these isolates were analyzed through bacterial analysis pipeline as CGE site. Multilocus sequence typing, resistant genes, plasmid incompatibility (Inc) typing, and plasmid sequence typing were also determined by CGE site.
3. Results
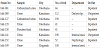
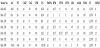
The proportion of blaCTX-M-55 positive E. coli was 12.5% (8/64) of the CTX-M-1 group ESBL genes positive isolates (Table 1). Two of eight isolates were from outpatient, and hkk-129 and hkk-130 were likely to be collected from the same medical facility. Among the 8 blaCTX-M-55 identified isolates, 7 isolates of E. coli were applied for further antimicrobial susceptibility and next-generation sequencing data. But, one isolate remaining was not available for re-growing from bacterial stock. The results were shown in Table 2 and Table 3. Four and six isolates were resistant to fosfomycin and ciprofloxacin, respectively. As a result, blaTEM-1B and tetA were detected in 6 and 5 isolates. Some aminoglycoside modifying enzyme genes were detected in 4 isolates. All isolates harbored plasmid incompatibility type (Inc) F plasmid. IncN and IncI1 were detected in 2 and 2 isolates, respectively. Additionally, E. coli sequence type (ST) 131 was determined in 3 isolates, and ST70, ST1193, ST1771, and ST2003 was identified in each of 4 isolates. The isolate of hkk-61 harbored IncF, IncX, and IncI1, and carried mphA, floR, and tetB that provide trimethoprim, florphenicol, and tetracyclin resistance, respectively. Moreover, the sequence type, resistant genes, and harbored plasmids of hkk-129 corresponded to those of hkk-130.
4. Discussion
This study reveals the prevalence and molecular characteristics of CTX-M-55 producing E. coli isolated from medical facilities with fewer than 300 beds in Kanagawa prefecture, Japan. There were many studies on the prevalence of CTX-M-55 producing E. coli in tertiary hospitals in Japan [12], but not in middle and small medical facilities. This study dealing with the strain isolated from medical facilities with less than 300 beds demonstrates precisely the prevalence of CTX-M-55 producing gram-negative bacteria in community in Kanagawa prefecture.
It is well known that CTX-M-15 producing E. coli is widely disseminated to the world. Nonetheless, it is surprising that the prevalence rate of blaCTX-M-55 positive isolate in CTX-M-1 group ESBL genes positive E. coli was greater than 10%. CTX-M-55 producing Enterobacteriaceae and its plasmids were isolated from livestock in China, Southeast Asia, and East Asia [13,14]. Shu et al. reported that CTX-M-55 producing Enterobacteriaceae was more common in community- and hospital-associated infection than CTX-M-15 in China [15]. Kameyama et al. also pointed out that CTX-M-55 was a secondary dominant type of CTX-M in Japanese broiler farms [16]. Therefore, it is suggested that the increment in prevalence of CTX-M-55 producing E. coli in human communities is due to its dissemination into livestock and retail meats.
The sequence type of E. coli harboring blaCTX-M-55 gene were diverse. Three of the seven isolates corresponded to E. coli ST131. E. coli ST131 harboring blaCTX-M-15 is disseminated to the world. It was reported, moreover, that E. coli ST131 harboring blaCTX-M-27 also spread in Japan [12]. Unfortunately, the spread of E. coli ST131 carrying blaCTX-M-55 gene may have the potential for dissemination of the strain that is resistant to ceftazidime. Two isolates, hkk-129 and hkk-130, were likely to be isolated from the same facility (Table 1), and are identical. This finding suggests that E. coli ST131 has a high risk of clonal spread in a facility and that continuous surveillance for the CTX-M-55 producing E. coli ST131 is needed.
One of the seven strains was recognized as E. coli ST1193. E. coli ST1193 harboring blaCTX-M-55 dominates in China, which differs from the result of this paper [17]. E. coli ST1193 and ST2003 were also reported to be isolated from clinical patients [18]. In this study, these two strains were resistant to ciprofloxacin (CPFX). Particularly, a number of literatures have addressed the E. coli ST1193 having resistance to CPFX. As can be seen from Table 3, plasmid mediated quinolone resistant genes (PMQR) such as qnr and aac(6’)-Ib-cr were not detected in any isolates. Hence, the resistance of CPFX in E. coli ST1193 seems to be conferred by the chromosomally mutation of quinolone resistant determined regions (QRDR) [19]. Meanwhile, there are few reports that the other ST, ST70 and ST1771, was that sporadically isolated from livestock and retail meats [19,20], and these strains were susceptible to CPFX. If the PMQR genes are acquired by these strains by means of horizontal transfer among veterinary fields, its spreading will be concern about the treatment using fluoroquinolone agants against several infections diseases such as pyelonephritis.
The resistant genes combined with blaCTX-M-55 were blaTEM-1B and tetA. This result is consistent with that of earlier studies [5]. Since the Inc type of plasmids harboring blaCTX-M-55 was IncF, N, and I, blaCTX-M-55 may be located on their Inc type plasmids in E. coli [21-23]. The resistant gene of floR responsible for resistant to florphenicol, which is generally used in a veterinary field, was detected from hkk-61. Meunier et al. suggested that florphenicol selects the strain producing β-lactamases in livestock [24]. Thus, the florphenicol and β-lactam co-resistance caused by floR and blaCTX-M-55 on the same plasmid then might be related to dissemination of the strain. In this study, however, it was uncertain which Inc types of plasmid encode each resistant gene, because the contigs were not assembled completely. Besides, it was unclear whether the strain possessed one or more than 2 plasmids.
Moreover, hkk-141 and hkk-199 involving fosA gene harbored IncN plasmid. MacGann et al. reported that IncF with blaCTX-M-55 and mcr-1 was determined in the strain isolated in US and that IncN plasmid coding fosA gene was retained simultaneously [25]. Additionaly, many reports in China described the determination of the fosA combined with IncN [26,27]. The spread of fosA possessing E. coli combined with blaCTX-M-55 may restrict therapeutic options for treatments of urinary tract infection (UTI) patients on which β-lactam has no therapeutic response. On the other hand, the fosfomycin resistant rate of E. coli isolates from community UTI was 0 %. This finding then confirms that fosfomycin is available as a candidate antibiotic agent to community-UTI patients [28].
5. Conclusion
This is the first study on the epidemiology and characteristics of CTX-M-55 ESBL producing E. coli isolates from regional medical facilities with less than 300 beds in Japan. As a result, CTX-M-55 producing E. coli originates from a different clone. The ST of isolates harboring blaCTX-M-55 in medical facilities, but not in central hospitals, was classified into several types including global clone ST131, but other STs of isolates from retail meats and livestocks was also determined. Unlike ST, the plasmid inc type in the clinical isolates corresponded to the type of the isolate from retail meats and livestocks.
The limitation and remaining question of this study is whether these strains directly spread to human through meat ingestion or not, that is to say, whether the strain transfers its β-lactamase genes to human strains through horizontal transfer. However, the occurrence of the floR gene detected from some isolates suggests that the dissemination of blaCTX-M-55 is related to veterinary fields.
Among the isolates possessing blaCTX-M-55, the resistance against fluoroquinolone and fosfomycin depending on spread of ST131 and/ or ST1193 and of fosA has a clinical impact to restrict therapeutic options against infectious disease such as community UTI.
Competing Interests
The authors declare that they have no competing interests.