1. Introduction
Heart failure is a leading cause of hospitalization. More than 915,000 new patients are diagnosed with heart failure, and the incidence increases with age, with 10 patients per 1000 population after 65 years of age suffering of heart failure in the United States [1]. Its prevalence is growing and estimated up to 1 in 5 among 65 years of age or older in 2030 for the Americans population [2]. Prognosis of heart failure is poor, and the death rate remains high. Age-adjusted 1-month and 1-year case fatality after hospitalized heart failure was 10.4% and 29.5%, respectively [3]. Up to 50% of people diagnosed with heart failure will die within 5 years [4,5]. Re-hospitalization is also frequent as high as 25% of 1-month after primary diagnosis of heart failure [6,7]. In addition, the cost for the heart failure patient care is high and growing. In 2012, total cost for heart failure was estimated to be $30.7 billion in America. Of this total, 68% was attributable to direct medical costs [8]. Projections show that by 2030, the total cost of heart failure will increase almost 127% to $69.7 billion from 2012. This equals ≈$244 for every US adult [8].
Once diagnosis of heart failure is made, it is recommended to determine the etiology and start treatment according to the etiology and pathophysiological status [9,10]. Comprehensive understanding of anatomy, function, and pathophysiological status in each patient is essential to provide optimal therapy [9,10]. Of incident hospitalized heart failure events, 53% had heart failure with reduced ejection fraction (HFrEF) and 47% had preserved ejection fraction (HFpEF). [3]. HFrEF has several therapeutic options to improve prognosis. On the other hand, HFpEF has no such treatment to improve survival. Therefore, these 2 groups should be managed differently in some way as appropriate [11]. Most required information can be obtained from non-invasive imaging modalities, such as echocardiography, magnetic resonance imaging (MRI), multi-detector computed tomography, and nuclear imaging. Each imaging modalities has its own strength and limitations (Table 1) [9]. The imaging modalities should be selected based on what kind of information is needed to manage each patient: etiology (ischemic/non-ischemic), function (reduced/ preserved ejection fraction and dyssynchrony), complications (mitral regurgitation and fatal arrhythmias). Among these information, the etiology is the most important issue because ischemia is one of the most frequent causes of heart failure and crucial for therapeutic selection.
Etiology of heart failure was investigated using meta-analysis fashion from 24 published study including 43,568 patients, of whom 62% had an ischemic etiology [12]. The cause of more advanced heart failure patients who were candidates for cardiac resynchronization therapy (CRT) was also reported. Among 14 observational studies including 3,463 patients, 1,842 (53.2%) patients had an ischemic etiology [13]. Therefore, ischemic etiology is a leading cause of heart failure. In patients with ischemic cardiomyopathy, advanced heart failure, and fatal arrhythmias, indication for revascularization, cardiac resynchronization therapy, and implantable cardiac defibrillator should be evaluated, respectively. For this purpose, non-invasive imaging is also useful.
Myocardial viability has been regarded as an essential element for indication of revascularization in patients with left ventricular (LV) dysfunctionand coronary artery disease (CAD). The utility of viability assessment was reported in a meta-analysis of 24 viability studies including 3088 patients by Allman et al. They showed strong relationship between viability and survival after revascularization (Figure 1)[14]. Schinkel et al. also reported the importance of viability determination in terms of prognosis. A total of 28 prognostic studies including 3848 patients were analyzed. The patients with viability who underwent revascularization demonstrated the lowest mortality rate (3.6%), whereas annualized mortality rate were not different between non-viable patients and viable with medical treatment patients (ranging from 9.1% to 11.6%) [15]. However, outcome after revascularization varies even in the presence of substantial myocardial viability. STICH trial was conducted to clarify the merit of coronary artery bypass grafting (CABG) in patients with HFrEF and less severe multi-vessel CAD. All-cause mortality was not reduced by CABG, however, cardiovascular death and death from any cause or cardiovascular hospitalization were significantly reduced (relative risk reduction rate was 19% and 26%, respectively) [16]. The next issue is who is benefit from CABG? Myocardial viability has been regarded as an essential element to select candidates for revascularization. However, the viability determination did not identify patients with a differential survival benefit from CABG as compared with medical therapy alonefrom the sub-study of STICH trial [17]. STICH trial recruited myocardial perfusion single photon emission computed tomography (SPECT) or dobutamine stress echocardiography (DSE) for viability determination. Therefore, viability might have been underestimated because of lower sensitivity to detect viability with these two modalities. However, F-18-fluorodeoxyglucose (FDG) positron emission tomography (PET), which is the most sensitive imaging to detect viability, assisted management for patients with severe left ventricular dysfunction and suspected CADalso failed to demonstrate a significant reduction in cardiac events compared with standard care (PARR-2 study) [18]. Therefore, myocardial viability assessment is controversial to select appropriate candidates for revascularization after STICH era.
This review focuses on myocardial viability and discusses whether myocardial viability assessment is crucial before revascularization.
2. Definition of Myocardial Viability and Pathophysiological Status
Myocardial viability is defined as myocardial segments characterized by reduced contractile function but potentially reversible either spontaneously or with revascularization. Left ventricular (LV) dysfunction had been regarded as irreversible before revascularization era. After introduction of the notion, “hibernation” and “stunning”, it has well established that dysfunctional but viable (hibernating or stunning) myocardium in patients with chronic CAD will considerably improve in function after revascularization [19,20].
Hibernation refers to the status of ischemic myocardium with reduced or absent wall motion but preserved cell viability. Myocardial perfusion may be normal or near normal at rest with diminished coronary flow reserve [21]. Stunning refers to the status of long lasting reduced myocardial contractile due to transient severe or repetitive ischemia that recovers eventually [22]. These dysfunctional but viable myocardium (jeopardized myocardium) can be determined by viability testing and recovers their function with revascularization. In contrast, mixture of intact myocardium (non-jeopardized) and scar tissue will not recover in function but still regarded as viable myocardium. Therefore, viability testing needssimultaneous assessing myocardial jeopardy in terms of functional recovery after revascularization.
3. Similarity and differences among imaging technique in determining viability
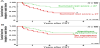
Multiple imaging modalities, including DSE, MRI, SPECT, PET have been used for assessing myocardial viability and prediction of outcome after revascularization. Sensitivity and specificity of various viability testing in predicting recovery of function are reported (Figure 2, Table 2) [15,23]. DSE is performed with stepwise infusion of dobutamine from 5 to 40 mcg/kg/min. Contractile reserve is assessed by wall motion improvement during low-dose phase (5 to 10 mcg/kg/min). Ischemia is also evaluated by deterioration of wall motion at high dose phase (10 to 40 mcg/kg/min). Biphasic wall motion response represents viable and ischemic myocardium. However, it has been reported that up to 50% of dysfunctional segments without contractile reserve still have resting perfusion (≥50% of % uptake in myocardial perfusion imaging) and/or glucose metabolism. This discrepancy means that DSE indicates no viability but nuclear imaging does. Therefore, some of these segments may improve function after revascularization. Hence, these 2 modalities are less sensitive but more specific to detect viability compared to nuclear imaging based on the “Ischemic Cascade” theory (Figure 2, Table 3)[15,23,24].
Nuclear imaging has been used widely and there is a lot of evidence among various viability testing. 201Thallium chloride (201Tl) reflects myocardial perfusion and cell membrane integrity. In addition to the conventional stress-rest protocol, rest-redistribution and stressredistribution- reinjection protocol are feasible. Viability is ascertained in case of redistribution in a region of dysfunction. Even in the absence of redistribution, ≥50% uptake indicates viability. Figure 3 demonstrates anteroseptal fixed defect with 201Tl and apical dyskinesis in patients with prior MI. Dyskinesis without redistribution implies no viability; however, %uptake remains ≥50% in the infarcted zone, except apex and adjacent anterior wall. After PCI to the severe stenosis of left anterior descending artery, both myocardial perfusion and LV function recovered to normal, including apex (Figure 4). Stress/Rest perfusion SPECT tends to underestimate myocardial viability (Figure 2); therefore, understanding the feature of each imaging modality for viability testing is essential and careful observation is crucial.
99mTechnetium perfusion tracers are also available. Retention of the tracers indicates cell membrane integrity and mitochondria function. Percent uptake ≥50% also indicates viability. In case of severe ischemia such as resting ischemia, sestamibi SPECT after nitrate administration is recommended so as to increase coronary blood flow (supply) to the compromised hypoperfused area. More than 10% increase in tracer uptake after nitrate administration indicates viability [25].
PET using fluorine18-deoxyglucose (FDG) is gold standard for viability assessment. FDG is a glucose analog and reflects glucose metabolism. FDG uptake depends on the metabolic circumstances. High blood glucose and low free fatty acid with high insulin level are required to obtain maximum uptake. This situation can be achieved by preparation such as simple oral glucose loading or hyperinsulinemic clamping [26]. FDG PET is assessed in combination with perfusion study, such as nitrogen13-ammonia PET and sestamibi SPECT. Perfusion reduction with preserved metabolism reflects hibernating myocardium recognized as “mismatch pattern”. Figure 5 demonstrates mismatch pattern in anteroseptal and inferior regions with 201Tl SPECT/18F-FDG PET imaging. Diffuse severe hypokinesis was observed with reduced LVEF (24%) and remodeling. Large hibernating myocardium with severely reduced EF and remodeling apparently indicated revascularization; however, this patient refused reperfusion therapy, resulted in cardiac death 20 months later.
MRI is used for viability determination with low dose dobutamine same as DSE with similar detectability (Table 3, Figure 2)[15,23,24]. MRI with delayed contrast enhancement is also useful. Kim et al. reported that wall motion recovery can be predicted with the degree of myocardial enhancement. As the degree of enhancement become thicker, there will be less chance to improve wall motion. Wall motion recovery cannot be expected in patients with myocardial enhancement exceeding 51% of its thickness [27]. On the contrary, preserved thickness without contrast enhancement can predict systolic function recovery. Ichikawa et al. reported that the dysfunctional zone with wall thickness ≥ 5.1mm in patients with prior MI and ≥3.9mm with acute MI without contrast enhancement can recover with revascularization [28].
4. Outcomes after Revascularization associated with viability
A sub-study of STICH trial demonstrated that the viability determination did not identify patients with a differential survival benefit from CABG as compared with medical therapy alone [17]. PARR-2 study was conducted in a randomized fashion to assess the effectiveness of FDG PET-assisted management in patients with severe ventricular dysfunction and suspected CAD. Unfortunately, this study also failed to demonstrate the usefulness of FDG PETassisted management for such patients [18]. However, sub-study of PARR-2 clearly demonstrated that ischemic cardiomyopathy with larger amount of hibernating myocardium have improved outcomes with revascularization [29]. LV remodeling also affects prognosis. Bo now et al. reported that absence of viability with LV remodeling (end-systolic volume index > 84 ml/m2) predicts the highest mortality regardless of treatment. However, combination of viability and LV remodeling did not influence the effect of CABG relative to medical therapy in STICH cohort [30].
Viability is important to predict LV dilatation after acute myocardial infarction. In patients with large infarct (peak creatine kinase > 1000 IU/l), viability assessed by low dose DSE was the only predictor of LV dilatation [31]. Even in the absence of EF improvement after CABG in chronic CAD, patients with viability have better prognosis compared with those without viability [14]. Classical definition of myocardial viability is myocardial segments characterized by reduced contractile function but potentially reversible either spontaneously or with revascularization. However, viable myocardium sometimes does not recover its systolic function after revascularization. Even in that case, prognosis may be better than the case without viability as long as concomitant jeopardized myocardium [32]. Mechanism of improvement of prognosis can be speculated as prevention of LV dilatation (remodeling). LV remodeling is also major predictor of prognosis in patients with CAD. Therefore, viability assessment is still important before revascularization even in the absence of EF improvement.
5. Additional factors regarding prediction of functional recovery
From the prognostic point of view, viability is not the only predictor.
Once viability is confirmed, timing of revascularization should be also taken into consideration. Early revascularization is beneficial in substantial viability; however, late revascularization is associated with worse outcomes in terms of LVEF improvement and mortality [33,34]. Long term mortality was 4-folfd higher in the later revascularization group (>1 month) than that in the earlier revascularization group (≤1 month) [33]. Therefore, recommended period for revascularization is within 1 month after viability testing.
Poor exercise capacity is another predictor of mortality. Stewart et al. reported that mortality was lower for patients randomized to CABG compared with medical therapy who walked ≥ 300m in 6 minutes in a sub-study of STICH trial (hazard ratio [HR]: 0.77; p = 0.038) Patients unable to walk 300m in 6 minutes or with a physical ability score ≤ 55 had higher mortality rate during first 60 days with CABG (HR: 3.24; p = 0.002) [35].
In the assessment of viable (hibernating) myocardium using PET, scar volume can be also quantified. Perfusion/metabolism mismatch is well-known parameter for viability; however, extent of scar tissue is negatively correlated with EF improvement after revascularization and a stronger predictor than perfusion/metabolism mismatch [36].
Extent of coronary and myocardial disease also affects the outcome. Presence of 3-vessel disease, EF < 27%, and end-systolic volume index > 79 ml/m2 are regarded major prognostic factors. Of these factors, patients with 2 to 3 factors had reduced long term mortality with CABG compared with those who received optimal medical therapy from the STICH cohort (HR: 0.53; p <0.001). On the other hand, CABG had no such effect in patients with 0 to 1 factor (HR: 0.88; p = 0.535). Therefore, more extent and more severe disease tend to be beneficial with CABG [37].
In addition to the viability status, these additional factors may influence the outcome. The COURAGE trial demonstrated that percutaneous coronary intervention (PCI) did not reduce mortality in patients with stable CAD compared with optimal medical therapy as a whole [38]. However, moderate to severe ischemic patients were proved to benefit from PCI from the nuclear sub-study [39]. Similar situation exists around the viability issues. Therefore, adjusting these factors indicated above is required before final conclusion.
6. Role of viability assessment
After STICH trial, viability testing before revascularization has been regarded as meaningless because inducible myocardial ischemia or viability does not identify patients with worse prognosis or those with greater benefit from CABG over optimal medical therapy [17,40]. Despite the consistent negative results for the viability testing, apparent limitations exist in these sub-studies. First of all, the no blinded and nonrandomized fashion for viability testing of only <50% of eligible patients introduces considerable selection biases. Second, revascularization was performed not guided by the presence of viable myocardium within the corresponding coronary artery territories. Third, viability testing was restricted to either SPECT or DSE, which are less sensitive to detect viability than MRI with contrast enhancement or PET [15,27]. In addition, resting ischemia is often observed in patients with severe myocardial ischemia. In such cases, summed difference (= ischemic) score may not reach as high as 4 with SPECT due to much poorer coronary flow reserve or balanced ischemia, and severe ischemic segments may not demonstrate contractile reserve in as high as 2 segments with DSE. Therefore, a randomized trial of viability guided revascularization versus optimal medical therapy after viability assessment using PET or MRI with contrast enhancement is necessary.
PARR-2 study failed to demonstrate the usefulness of FDG PETassisted management for patients with severe ventricular dysfunction and suspected CAD. [18] However, sub-study of PARR-2 demonstrated that ischemic cardiomyopathy with larger amount of hibernating myocardium have improved outcomes with revascularization. Those with hibernating myocardium >7% had a significantly reduced composite primary endpoint including cardiac death, myocardial infarction, and cardiac hospitalization with revascularization compared with medical management (3 [13%] vs. 9 [56%], p = 0.015) [29]. Another sub-study of PARR-2 trial revealed that FDG PET-assisted management significantly reduced the same endpoints with revascularization compared with standard care in experienced centers having heart teams (19% vs. 41%, p = 0.005) [41]. Inaba et al. demonstrated that similar survival benefits with revascularization of viable myocardium regardless of imaging technique used to determine viability in a meta-analysis. However, cutoff value of viable myocardium extent for each modality should be separately determined. Sensitive modality such as PET revealed relatively lower cutoff value compared with less sensitive DSE and SPECT (Table 2) [42] .
In predicting favorable outcomes after revascularization for CAD patients with LV dysfunction,accurate viability testing with jeopardized myocardium assessment and management with reliable heart team may be required.
7. Viability and Cardiac Resynchronization Therapy
Cardiac resynchronization therapy (CRT) is effective to improve outcomes of advanced heart failure regardless of ischemic or nonischemic etiology [43]. However, about 30% of these patients did not respond to CRT [44]. General indication for CRT required 4 factors: refractory to medical therapy, NYHA functional class II-IV, with LVEF < 35%, and QRS duration > 120 msec [9,45,46]. To reduce non-responders, some methods which can discern who is benefit from CRT is demanding. Left ventricular mechanical dyssynchrony is prevalently assessed by echocardiography using tissue Doppler imaging technique and may be one of the potential predictors for response to CRT. PROSPECT study is a prospective 53 multi-center study including 498 patients who fulfilled standard indication for CRT and conducted whether 12 parameters of mechanical dyssynchrony derived from echocardiography can differentiate between responders and non-responders to CRT. Unfortunately, no single parameter of dyssynchrony could predict the response to CRT because of wide variability of the results [47].
Nuclear imaging also provides mechanical dyssynchrony parameters [48]. In contrast echocardiography, nuclear imaging technique is less variable and determined the responders to CRT more accurately [48]. In addition, the extent and location of scar tissue can be determined [49-51]. Phase analysis of gated SPECT data determined the onset of mechanical contraction by measuring regional count variation over cardiac cycle, which is consistent with wall thickening, with Fourier transformation [52]. Phase standard deviation and the phase histogram bandwidth predict response to CRT (Figure 7) [48]. Responders demonstrated larger histogram bandwidth (94 ± 23° vs 68± 21°, p < 0.01) and stander deviation (26±6° vs 18±5°, p < 0.01). Cutoff value of 102.5° for histogram bandwidth and 19.6°for phase SD demonstrated that sensitivity, specificity, and area under the curve(AUC) for predicting response to CRT were 83%, 81%, and 0.83; 83%, 81%, and 0.85, respectively [48]. These dyssynchrony parameters derived from gated SPECT were superior in predicting response to CRT than those obtained by echocardiography demonstrated in PROSPECT study (AUC ≤ 0.62) [47]. Another predictor of responders to CRT is extent of scar tissue and viable myocardium. [49,53,54,55] Summed rest score (SRS) is quantified as an index of scar extent on myocardial perfusion SPECT. SRS ≥ 27 predicts lack of response to CRT (Figure 8) [48]. Pacing site and degree of localized scarring also affect the response to CRT. The latest activation region is the most appropriate site for LV lead placement and associated with good response to CRT [55,56]. Localized scar burden at pacing site also affects the response to CRT. [49,57,58].
CRT responders can be identified from comprehensive evaluation including LV mechanical dyssynchrony, scar burden/residual viable myocardium, concordance of pacing site and the latest activation region, and localized scar burden at pacing site. All these information can be obtained from gated myocardial perfusion SPECT as one stop shop which is less variable and reliable modality.
8. Conclusion
Ischemic heart failure patients need comprehensive evaluation including etiology, function, and pathophysiological status for optimal management. Multi-modality imaging can provide most of these information. Of these, ischemia and viability are particularlyimportant.Viability alone may not predict who benefit from revascularization. However, integration of viability, concomitant myocardial jeopardy, scar burden, and other relevant information leads to accurate prediction who benefit from revascularization. After completion of comprehensive understanding of the individual heart failure status, personalized management with heart team will maximize the efficacy of each treatment.
Competing Interests
The authors have no competing interests with the work presented in this manuscript.