1. Introduction
Perinatal Asphyxia is the second largest contributor to global neonatal mortality rate (NMR). It accounts for 27% of NMR in Nigeria and is a major cause of disability despite public health interventions targeted at its reduction in the past four decades [1,2].
The burden of Perinatal asphyxia (PA) in Nigeria is assuming epidemic proportions [2]. The typical presentation is failure of the new-born to resume or sustain spontaneous respiration after complete delivery with hypoxaemia, hypercapnia and acidosis [3,4].
Survivors present several short and long term morbidities, including: seizure disorders, tone abnormalities, feeding difficulties, delayed developmental milestones, learning difficulties, cerebral palsy and mental retardation. The morbidities increase with asphyxia severity. The frequency of the most severe complication, hypoxic ischaemic encephalopathy (HIE), incidence of up to 26.5/1000 live births is unacceptably high despite advances in perinatal care [5,6]. This is many times the international incidence of 2-6/1000 live births [7].
Perinatal asphyxia leads to excessive release and reduced uptake of glutamate in the newborn brain. Increased glutamate concentrations open N-Methyl-D-Aspartate (NMDA) channels allowing excessive calcium influx into the neurons and causes irreversible neuronal injury [8,9]. Magnesium is a naturally occurring NMDA receptor antagonist that blocks neuronal influx of calcium within the ion channels [9,10]. Without interruption of calcium influx, neuronal injury or death is the result, manifesting either as mortality or survival with sequelae; hence the neuroprotection strategy [7].
Magnesium sulphate may also have direct actions on mitochondrial activity, anticonvulsant properties and haemodynamic effects by increasing cerebral blood flow. Some data also suggest that MgSO4 may serve an antiapoptotic role and prevent neuronal cell loss [11-13].
More recently, attention has been drawn to many pharmacologic agents with anti-inflammatory and neuroprotective properties. These include erythropoietin, melatonin, magnesium sulphate (MgSO4), topiramate, xenon, and allopurinol [14]. These agents have specific pathways in the pathophysiology of perinatal asphyxia. Antioxidants have also been tried in animal models for the prevention of post asphyxia brain injury syndrome [15-17]. These have provided evidence that led to the different trials with antioxidants or their combined use with other modalities of therapy [18-20]. In fact, the clinical use of Magnesium sulphate to counteract the effect of glutamate and provide additional pharmacologic neuroprotection to hypothermia in the Mag Cool study is one of such [21]. Similar experience has also been extended to the use of Magnesium sulphate and antenatal corticosteroids for preterm mothers [18].
Treatment of perinatal asphyxia in Nigeria is largely symptomatic and supportive despite new beneficial treatment modalities and experimental therapies [7]. These are of prohibitive unaffordable cost in resource limited environments moreover they are not accessible to practitioners given the strict protocol and inadequate supportive care required for administration of therapeutic hypothermia [22-24].
The neuroprotection properties of magnesium sulphate (MgSO4) have been documented in several animal studies [10,25-28]. Magnesium has also shown beneficial effect in reducing cerebral palsy in infants of mothers that received prenatal magnesium sulphate for other perinatal indications [29]. Its usefulness in the management of persistent pulmonary hypertension of the newborn, one of the common comorbidities associated with perinatal asphyxia may be an added advantage and usefulness in resource limited setting like ours [30,31].
Magnesium sulphate was shown to improve neurologic outcome of severely asphyxiated newborns in a randomized, placebo controlled trial, which is in tandem with previous observational studies which advocated for more studies and multicenter trials [32]. This low cost, low technology, readily available intervention could be a possible coping strategy for stemming the tide of perinatal asphyxia and hypoxic ischemic encephalopathy in low resource settings.
2. Subjects and Methods
This study was conducted at the neonatal unit of University of Benin Teaching Hospital, Benin City, a tertiary public health facility in Southern Nigeria. The unit stores data of previously managed cases in her data base and utilises standard protocols and guidelines for management of different morbidities. These are updated and reviewed regularly. Since 2013 December, the unit has strengthened her capacity for respiratory support and offers respiratory support to babies when indicated. The unit has a capacity of 50 admissions: 32 cots and 28 incubators.
Records of 611 pre-magnesium treatment era cases of perinatal Asphyxia admitted and managed in the unit from July 2009 to December 2014 were scrutinized to identify their gestational maturity and their HIE stages. These historical controls, constituted the comparison group against who the magnesium sulphate treated cases were compared.
The Institutional Ethical committee approved the protocol for the use of MgSO4 in perinatal asphyxia cases. The parents of such infants were appropriately counselled: the essence of the study was explained. Parental consent was obtained before enrolment of asphyxiated babies.
All babies from both the deliveries in the labour suites, labor ward theatres (inborn) and babies born before arrival (outborn) referred to the hospital for care are recruited. Eligibility criteria were: babies with history of foetal distress, meconium stained amniotic fluid requiring resuscitation with bag-mask-valve device or endotracheal intubation during resuscitation; Apgar score of ≤3 or < 7 at one and five minutes and presence of signs of HIE; metabolic acidosis, multisystem organ dysfunction [33]. Babies born before arrival were recruited when there is history of prolonged labour, difficult delivery, poor or no cry at birth or evidence of features of HIE and or multisystem organ dysfunction. Babies of mothers who received antenatal MgSO4 and infants with obvious congenital anomalies or features of congenital heart disease were excluded from the study.
A semi structured questionnaire proforma was used to document the socio-demographic details, antenatal, intrapartum information and physical features of recruited babies. Those with HIE were classified according to the staging system proposed by Sarnat and Sarnat [34].
MgSO4 was administered within half hour of admission at 250mg/ kg/dose by slow intravenous infusion over 15-30 minutes [32] every 24 hours for total of three doses. Supportive care (respiratory, inotropes, etc.) was provided as required by the baby and documented. Treatments for other comorbidities were according to the unit protocol. The neurologic changes were documented on the proforma over ten days of admission or until they are normal.
Data were analysed as frequencies, chi square using IBM SPSS Statistics [20]. The level of significance, p value was set at <0.05.
3. Results
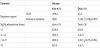
Nine hundred and fifteen babies were admitted: 474 inborn admissions and 2582 deliveries occurred over the study period. This gives an incidence of 20.1 and 13.8 per thousand for PA and HIE respectively. The general characteristics are shown as (gender, weight categories, gestational age (Table 1): booking status, place of birth, Mode of delivery, Neonatal unit placement (Table 2). Examination of the neonatal unit admission placement showed a trend of more outborn (42.5%) presenting with HIE stage III versus inborn (21.1%); whilst more of the inborn (36.8%) were in HIE stage I and 42.1% of inborn and 45% of presented in stage II. Table 3 depicts the mode of management of these babies with respiratory support, magnesium sulphate and their outcome. Sixty percent of these babies received respiratory support as shown in Table 2. The CPAP mode was the most common respiratory support and was associated with higher survival rate. Irrespective of the time of initiation of magnesium sulphate, survival was improved. Eighty three percent of the recipients survived.
There were 100 asphyxia cases: 52 inborn and 48 outborn. The Perinatal Asphyxia rate was 10, 93% hence the incidence of 20.1 per 1000 live births. The HIE rate was 78% giving an incidence of 30.2 per 1000 live births; the highest HIE stage (38%) gives an incidence of 14.7 per 1000 live births presenting in HIE II category followed by 25% or 9.7 per 1000 live births in HIE III category.
The significant contributors to survival of asphyxiated babies treated with MgSO4 were observed in HIE stage II & III (4.8615, p= 0.027) and the respiratory supported group. Gender, gestational age, booking status and neonatal unit placement were not significantly associated with survival.
Total admissions to the unit from July 2009 to December 2014 (comparison group) were 4088 and 611 were asphyxiated. One hundred and seventy four (28.5%) of these babies died relative to the seventeen (17%) of the Magnesium sulphate treated cases, p= 0.016. Four hundred and fourteen of the 611 PA cases had various degrees of HIE: stage I, was 73, stage II, 157 and stage III, 184. One hundred and sixteen (63.04%) of the stage III comparison group died relative to the ten (40%) of the treated HIE III group, p =0.027; 28.3% of all stages of HIE also died relative to the seventeen (17%) of the treated group, p= 0.016.
Table 4 shows the comparison of the historical controls with the MgSO4 treated groups in their respective categories. There was a significant difference in mortality between the comparison group and the MgSO4 treated group (p<0.05).
4. Discussion
The key findings of this study was the burden of perinatal asphyxia shown by overall incidence of 20.1 per 1000 live births (5.7%) and an HIE incidence of 13.7 per 1000 live births with 9.2 per 1000 live births presenting in HIE II and III categories. Survival of babies that received postnatal Magnesium sulphate was 83% and a mortality rate of 17% with significant difference in survival among those presenting in HIE II & III category. There was a significant difference in perinatal asphyxia, HIE and severe HIE survival between the comparison group and the MgSO4 treated group.
Respiratory support (CPAP & MV) significantly improved survival of babies that received Magnesium sulphate. The reason for the observed improvement might not solely be explained by the haemodynamic effect of magnesium sulphate. It might also be due to the combined effect of the respiratory support which further improved oxygenation and resulted in enhanced ventilation to perfusion ratio. Booking status, gestational age, neonatal unit placement and timing of MgSO4 administration were not contributory to the survival of these babies. The apparent lack of relationship between timing of administration of magnesium sulphate and survival might be explained by the difficulty in identification of the exact timing of the 6 hour therapeutic window period. The longer term outcome of the baby (beyond survival) as it relates to the time of intervention might be a better pointer to the efficacy of the neuroprotection offered by postnatal MgSO4.
The relationship between the time of commencement of magnesium sulphate and survival showed no significant relationship. Perinatal asphyxia deaths rates dropped from a mean incidence of 45% to 17% during the course of this study, which is an 85% reduction.
The burden of perinatal asphyxia of 20.1/1000 live births and combined HIE II & III incidence of 9.2 per 1000 live births recorded in this study is unacceptably high as it is 3-5 times the international incidence of perinatal Asphyxia and HIE [7].
The incidence of perinatal asphyxia and HIE II & III from this study however is slightly lower than 26.5/1000 live births and 12.1/1000 live births reported by Airede [6] in 1991 at a tertiary referral hospital in Jos, Nigeria. The reason for the difference may not be apparently evident as the locations do not share similar demographics. This finding could be a reflection of the slow improvement in neonatal care in Nigeria. The finding of a lower rate of moderate to severe HIE (II & III) is noteworthy and maybe due to improved referral of babies, better health seeking attitude of parents of sick babies affected by perinatal asphyxia and improved access to perinatal healthcare in this locale.
The findings of this study is indicative of tedious improvement of newborn healthcare in the population almost three decades after the Jos study. This is also reflected on the national neonatal mortality rate which has not improved significantly within the same period. It is also of note that the contribution of perinatal asphyxia to the national newborn mortality rate has remained largely unchanged over the past four decades and the economics of health has deteriorated significantly in the past four decades. Perinatal asphyxia therefore is still a major contributor to perinatal mortality and morbidity, hence the quest for better treatment solutions to reduce the high burden in resource constrained environment is germane.
It is of note that more of the babies with HIE III were referred, reflecting the danger of late presentation and delayed access to optimal newborn care. Adequate and focussed antenatal care, the presence of skilled birth attendant at deliveries and availability of resuscitative equipments are some of the factors that could forestall perinatal asphyxia in peripheral hospitals.
The survival of babies that received postnatal Magnesium sulphate from this study was 83%, a mortality rate of 17%. This mortality rate is higher than 10% reported by Bhat et al. [32] in India from the randomized placebo controlled trial (RPCT) of magnesium sulphate on perinatal asphyxia. The higher mortality rate from this study is noted and may be due to inclusion of preterm babies (16%) in the study population. The RPCT by Bhat et al. was on babies’ ≥37 week gestation and this age group had a comparable mortality rate of 12% from this study. The observed reduction in mortality and enhancement of survival might all have resulted from the combined result of cardiovascular, anti-inflammatory and anti-apoptotic actions of Magnesium sulphate. This reduction in mortality from magnesium sulphate could stem the tide of perinatal asphyxia epidemic in low resource settings.
Although the use of historic controls would appear to be a limitation of the study on its own because of the inherent pitfalls that retrospective reviews could be fraught with. The extent of affectation to the study has been limited by the fact that a robust record of asphyxiated babies has largely been well maintained. The use of these historic controls on the other hand has enabled access to a large pool of data of babies with perinatal asphyxia over time in the same facility. This has highlighted the fact that the asphyxia rates have remained high over time. The data also strengthened the case for the observation of improved survival of the magnesium sulphate treated group. This finding is contrary to the observation from other studies [34,36] who could not prove the positive effect of MgSO4 on mortality in the management of PA.
Nonetheless the long term outcome of the babies who received this treatment requires careful evaluation. The immediate positive short term outcome might have resulted from the anti-inflammatory effect of this therapy [15-17] which limits the antioxidant and reactive oxygen species release of the neurons and offers protection from immediate neuronal injury. It is certain that more evidence needs to be generated by further experiences with the use of anti-inflammatory agents post PA, and the simplest pharmacological agent which has wide and ready accessibility to LRS settings is magnesium sulphate.
We report an overall mortality rate of 17% and 12% for the term babies from this study. This is similar to the 10% reported by by Bhat et al. [32]. It is however less than 44% from the National Institutes of Child Health and Human Development (NICHD) for the Whole- Body Hypothermia for Neonates with HIE by Shankaran and colleagues [22]. This study unlike the observations of the NICHD that was focused on HIE with moderate to severe impairment at 18-22 month follow-up [22] included all categories of babies who received postnatal magnesium in the newborn period. While cooling is the standard of care in developed countries, it is not yet a treatment modality in Nigeria. The absence of this modality of care may be due to unavailability of the cooling infrastructure in any Nigerian hospital. It may also stem from the high cost of cooling equipments and strict protocol for their use. There is however no comparative trial on therapeutic cooling and MgSO4 therapy.
The short term outcome for survival showed a significant difference among those presenting with HIE II & III. Up to 60% of babies in HIE III survived in contrast to 100% mortality at some quarter in the historical controls.
The significant impact of respiratory support on the use of magnesium sulphate for perinatal asphyxia babies is one of the key findings in this study. That 60% of asphyxiated babies had respiratory distress requiring support is of note and has been reported as one of the morbidities requiring respiratory support intervention [37,38]. Outborn babies had more mechanical ventilation requirement, while inborn babies benefitted more from nasal CPAP. This may be related to the late presentation of outborn babies in severe respiratory distress and HIE III category.
Respiratory distress is a feature of perinatal asphyxia and HIE arising from depression of respiratory centre, [39] acute respiratory distress syndrome, [40,41] persistent pulmonary hypertension of the newborn and meconium aspiration syndrome [42]. Respiratory distress and apnoea are common features hence the need to support them during the acute phase of the illness. The 60% reported in this study is lower than 78% reported by Gluckman et al. [43]. The respiratory depression and apnoea from magnesium sulphate administration was minimised by increased time of administration of MgSO4 used in this study.
There was no significant relationship between time of commencement of MgSO4 and survival. This is a key finding of this study as it differs from the 6th hour cut off point for intervention used by Bhat et al. and therapeutic cooling protocols [32,21,22]. The first six hours is the therapeutic window for intervention in perinatal asphyxia following the primary energy failure which occurs within minutes of the hypoxic-ischaemic insult. Within the therapeutic window, immediate adaptive factors are activated; with reperfusion including sodium overload and associated excitotoxicity, calcium overload and reactive oxygen species. These would cause immediate neuronal death if uninterrupted by therapy and usher the secondary phase of energy failure [7-9]. It is however difficult to know the precise time of onset and resolution of primary energy failure in newborns with HIE, hence we elected to treat all irrespective of their time of presentation. The implication of our finding particularly for our environment where there is delayed presentation of patients to hospital offers potentials for its use and further exploration of the benefits of its use for the late presenting patients. We found no relationship between the time of commencement of MgSO4 intervention and mortality. This is an area needing further investigation. Population education on asphyxia prevention and early presentation is key to stemming the tide of mortality and morbidities in survivors in our peculiar environment.
The line graph aptly summarizes the mortality trends before and during Magnesium sulphate use in the newborn unit. The perinatal asphyxia death rate plummeted from 45% before to 17% during the intervention. The HIE death rate also dropped from 40-60% to 10- 30% during the intervention while the HIE 3 death rate hovered at 0-60% from 50-100%. While the sustained decline in perinatal asphyxia mortality may be ascribed to the dual impact of respiratory support and magnesium sulphate administration, it is important to note that respiratory support alone would not bring about a sustained decline in mortality as shown by the sharp decline in September 2014 coinciding with its commencement in the unit. The reason for the rebound in mortality trends with respiratory support services alone is not readily apparent. The sustained decline in mortality from perinatal asphyxia and HIE by the dual implementation of respiratory support services and magnesium sulphate intervention needs further exploration and could be the subject of a multicenter study in Nigeria.
Competing Interests
The authors declare that they have no competing interests.
Author Contributions
Conceptualisation of the study: AAO
Development of Study design: AAO/ IkRO
Coordination of study: IkRO / AAO
Acquisition of data and Final Analysis: IkRO / AAO
Write up of first draft of Manuscript: IkRO
Write up of final manuscript: AAO IkRO
Agree with manuscript results and conclusions: AAO, and IkRO
Acknowledgments
The authors received no financial support towards this work but wish to gratefully acknowledge the superlative care provided by the neonatal unit nurses to these babies as well as the support of the large number of resident doctors who on a continuous basis cared for these babies. The authors acknowledge the support of Dr Oriafo who helped with searching for some of the references while the work was being conceptualized.