1. Introduction
Ectopic thyroid (ET), a form of thyroid dysgenesis, is a rare developmental, congenital aberration resulting from the abnormal migration of the thyroid gland during its passage from the floor of the primitive foregut to its final pretracheal position [1,2]. Thyroid dysgenesis accounts for 80–85% of permanent congenital hypothyroidism cases (CH). Nearly 60% of thyroid dysgenesis cases are due to ET [3], which is nonetheless rare condition affecting only 1: 100,000–300,000 individuals in the general population [4,5].
ET is detected by neonatal mass screening in some patients presenting hypothyroidism as neonates. In other cases ET is diagnosed later when signs due to enlargement of the mass, such as dysphagia, dyspnea and hemoptysis, begin to appear. A certain number of cases are also reportedly found incidentally during autopsies.
Herein we report a patient with dual ET, who started thyroid hormone replacement therapy at age 25 year.
2. Case report
The patient, an 8-year-old female, was referred to our hospital with the chief complaint of a mass in the anterior neck. She was the firstborn child of healthy, non consanguineous parents. A neonatal mass screening for thyroid function was negative. She had no signs due to hypothyroidism, such as developmental delay, growth failure or inactivity. At age 4 year, a mass was noted in her anterior neck, which was initially thought to be a median cervical cyst. Biopsy revealed the mass to be ET. It was monitored until age 8 year, when the mass became enlarged. The mass was soft, 1.3 cm in length, 2 cm in width, and situated on the right upper edge of the thyroid cartilage. The patient was euthyroid: the TSH level was 3.53 μU/ml (normal: 0.50- 5.00 μU/ml) and the T4 level was 7.03 μg/dl (normal: 6.10-12.4 μg/dl). Both thyroglobulin antibody and anti-thyroid microsomal antibody tests were negative. CT and 123I scintigraphy revealed dual ET, i.e., the thyroid tissue was divided into two parts, one part situated in the lingual root and the other on the thyroid cartilage.123I 24 h up-take was 39% (normal: 10-40%).
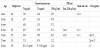
Table 1 shows the patient’s clinical course. Levothyroxine (LT4) was not administered at the patient’s initial visit to our hospital. Her growth spurt began around age 9 year. Her TSH level increased to nearly 10 μU/ml while her T4 level remained in the normal range at age 10 year. She had menarche at age 11 year and 4 month. A TRH test was performed at age 16 year when the patient’s T4 levels decreased to 6.19 μg/dl, nearly the lower limit of the normal range. It showed no excess TSH response in spite of the mildly elevated TSH. The mass had gradually enlarged until age 25 year when the TSH level began increasing again. The cervical mass size was now 3 cm in length and 4 cm in width. The TRH tests showed the peak TSH level at the time to be 40.1 μU/ml, which was higher compared to that at age 16 year. Therefore, LT4 25 μg was started and the volume of the mass decreased as a result of this treatment. The patient has continued to receive at the current dose of 32 μg/day. The patient did not show any signs due to enlargement of the mass, such as dysphagia or dyspnea, until she reached the age of 35 years.
3. Discussion
Our patient passed neonatal mass screening for negative and showed late-onset hypothyroidism. The high level of TSH and enlargement of the mass in the anterior neck improved after low-dose thyroid hormone replacement therapy was begun at age 25 year.
The clinical manifestations of ET are quite variable (Table 2) [5-9]. The age range at diagnosis is wide (2 month to 85 year). Most ET cases present as a single mass in the lingual position with no other thyroid tissue, but 9% of cases present dual ET [10], as in our patient. Interestingly these data were mostly reported from countries where mass screening was not done, suggesting the majority of ET cases could have been detected using a neonatal screening test. However, the results of the screening test in our patient were negative.
There have been several reports on the onset of dual ET. Agarwal, et al. reported a case of late-onset dual ET as in our patient [11]. Meng, et al. reported that hypothyroidism in dual ET was late-onset and mild. In dual ET, the age at onset tends to be higher (14.33 ± 8.69 vs 2.45 ± 1.11 year; p<0.01), the free T4 levels tend to be higher (12.07 ± 2.45 vs 7.78 ± 2.76 pmol/l (normal: 11.50-23.50 pmol/l); p<0.01), and the TSH levels tend to be lower (22.17 ± 25.97 vs 98.68 ± 59.98 μU/ml; p<0.01) compared to single ET [4]. Theoretically, thyroid function in ET depends on the volume of normal, functional thyroid tissue. Dual ET may have a larger functional thyroid tissue volume than single ET, which could explain the late-onset of hypothyroidism as seen in our patient. Indeed the present case showed an enlargement of the ET of the neck during puberty when the demand for thyroid hormone, in general, increases. Her subclinical hypothyroidism continued and thyroid hormone replacement therapy was started from the age of 25 year.
The differential diagnosis of the enlarged mass in our case was modular goiter, adenoma, Hashimoto’s thyroiditis, colloid goiter, and thyroid cysts, which can occur in the ectopic thyroid glands as well as in the orthotropic thyroid gland and lead to thyroid dysfunction [6]. However, these possibilities were low since the thyroid antibodies were negative in our case and the mass size correlated with the TSH level and decreased after replacement therapy was begun.
In conclusion, the ectopic thyroid should be carefully followedup even when asymptomatic because the clinical course can be lateonset, especially in patients with dual ET.
Competing Interests
The authors declare that they have no competing interests.