1. Introduction
Burnout syndrome was first described in the 1970’s work related constellation of symptoms that usually occurs in individuals without any prior history of psychological and psychiatric disorders. In many cases burnout is triggered by a discrepancy between the expectations and ideals of the employee and he actual requirements of their position [1]. The risk factors for burnout can be divided into two categories- (1) Individual related risk factors such as having poor self-esteem, maladaptive coping mechanism, unrealistically high expectations, and financial issues. (2) Organizational risk factors- conflict with coworkers, heavy workload, rapid institutional change, diminished resources and variability in work schedule. Burnout is a growing problem and it rose in nearly all specialities and it has high prevalence. According to American Psychiatric Association as estimated 40 % of psychiatrists have professional burnout. Emergency medicine had the highest greater than 60%. Among General practitioners the prevalence rate is 40% to 60% [2,3].
Research suggests that medical school burnout is estimated around 50%, about the same prevalence as in residents and physicians [4]. Consequences of medical student burnout, in addition to high levels of perceived stress and emotional distress, include self-reported cheating and dishonest clinical behaviors, increased symptoms of depression, and the increased likelihood of suicidal ideation [6,2,5].
In 2011, the prevalence of burnout among practicing physicians in the United States was estimated at 54% [3] with several contributing factors ranging from excessive workload to conflicts with worklife integration. This chronic condition not only impacts physician and medical students’ well-being but is also important because it is directly linked to lower patient satisfaction, longer post-discharge recovery time [6], and higher mortality ratios in hospitalized patients [2]. While the problem of physician burnout is widely recognized with diverse solutions implemented across the country, research into resident burnout is less, and there has been almost no research into medical student burnout.
2. Objective
To evaluate the prevalence of burnout and associated factors with the development of burn out among third year medical students at HBCU.
3. Methods
This study is approved by Howard University IRB. This is a crosssectional quantitative study Conducted at the Howard University Hospital from March 2018 to June 2018. The Howard University Hospital was built on the foundation of Freedmen's Hospital and Asylum, which cared for freed, disabled, and aged blacks. In 1868, after the Civil War, Freedmen’s Hospital became the teaching hospital of Howard University Medical School. In 1909, a new 278-bed Freedmen's Hospital was erected. In 1975, the current and modern University Hospital was opened. For many years, Howard University was the only Carnegie I research intensive institution and has trained more African Americans with professional or doctoral degrees than any other institution.
The study was performed in accordance with the international ethical standards of the Declaration of Helsinki. Medical students indicated their agreement to participate in the study via the electronic informed consent included in the electronic survey form. In order to ensure and facilitate the completion of the questionnaires and increase the confidentiality of the data, we chose to collect online questionnaire responses using the Survey Monkey program, which was obtained legally from the registration on the site (https://pt.surveymonkey. com).
4. Instruments
The questionnaire was designed to take on average of 15 minutes to complete and contained the following instruments.
4.1 Maslach burnout inventory (MBI)
22 item self-administered anonymous online survey which was distributed to all third-year medical students at HUH in Washington DC. The survey contains standardized questions from Maslach Burnout Inventory (MBI) to screen for the level of burnout in students, in combination with demographic and brief psychiatric history questions from the participants. The MBI instrument containing 15 unique items for the evaluation of burnout among medical students.
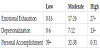
MBI analyzes burnout in three sub-scales on a continuum: Emotional Exhaustion, Depersonalization, and Personal Accomplishments. It divides the level of burnout into low, moderate and high for each of the three sub-scales. Higher scores on the Emotional Exhaustion and Depersonalization corresponds to higher levels of burnout and on the other hand lower scores in the Personal Accomplishments indicates a more severe burnout. The specific score ranges are reflected in the chart below.
A total of 105 third year medical students were invited to participate via a Howard University School of Medicine listserv and 61 people responded to the survey (participation rate of 58 percent).
5. Results
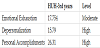
The level of burnout in HUH Third Year Medical students are as follows:
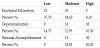
More specifically the number of respondents in each level of burnout in each category is being reproduced in the table below.
Our data suggests that most of the respondents show moderate and high levels of burnout. This study should act as a caution regarding the future physicians who are currently suffering from moderate to high levels of perceived burnout. If appropriate steps are not taken to intervene, the future negative impacts of burnout would be inevitable as described above.
6. Discussion
In this study, we investigated severity of burnout among third year medical students. Our data suggests that more than 60% of participants suffer from moderate to high levels of emotional exhaustion, above 80% indicated depersonalization at the same severity level and almost all the participants are not satisfied with their personal accomplishments which is leading to a burnout prevalence of above 70 percent in our participants. Our data suggests no difference in prevalence of burnout based on gender; however, prior diagnosis of a psychiatric illness was a major contributor to burnout levels in the severe level.
Physician burnout may be related to chronic workplace stressors starting as early as the first year of medical school, with onset of burnout arising from mental and physical exhaustion owing to the demanding medical curriculum, increasing time constraints, and harsh learning climates [3]. Calls for changes to medical curricula to address psychological distress have been made, but little is known about how curricula could be reformed and the expected outcome, despite information regarding the interference of burnout with the teaching/learning process. Other contributors to burnout are students’ self-perception of health, optimism and motivation regarding their studies, constant exposure to sick patients and death, and exhausting study routines [1].
Further, there are several negative consequences of burn out and depression such as difficulty relationships with co-workers, poor judgment or errors in patient care. Poor quality of care delivered to patients resulting in poor health outcome. Burnout also leads to lower retention of healthcare providers.
In order to minimize the negative consequences of depression and burnout syndrome, protective strategies have been reported in the literature such as physical activity, adequate sleep, psychosocial support and better learning environment [7]. It is crucial to develop strategies to prevent burnout and depression among students through curricular flexibility, better educational strategies, and schedule management are some of the promising ways to reduce burnout. Further, academic institutions should also consider the implementation of faculty development programs to optimize the learning environment [2].
Two key maladaptive coping strategies, avoidance and decreased engagement in values-based behavior, has been recognized to have a significant detrimental effect on medical students’ emotional well-being [1]. Strategies in managing these detrimental behaviors have been suggested in an effort to control the burnout level in this group. Avoidance is an attempt to prevent exposure to unwanted experiences and that provides immediate relief and satisfaction. However, this can also result in abandoning the medical student’s life goals. Dissatisfaction with life correlates with burnout in a variety of samples of health care providers [5].
The second factor, decreased engagement in values-based behavior, occurs when students engage in maladaptive actions even in the presence of dissatisfactory internal experiences. For example, students will over-study for exams thereby jeopardizing their relationships with friends and family members.
Burnout and depression can potentially be minimized if students are able to live in accordance with his or her values, despite stressors. This will provide opportunities to reconnect with the surrounding environment and benefit from social support and positive reinforcements and this will result in positive outcomes, including decreased psychological distress, better adjustment, and improved quality of life [8].
Contributors outside the school environment, and family-related stressors, have relatively insignificant influence on the development of burnout and stressors induced by the intense study, the frequent testing that takes place, and the continuous interaction with sick patients and death. If students spent more time outside of the hospital setting, this could potentially be protective against burnout. Family closeness and interactions have been reported as protective factor that lower stress levels and promotes happiness [8].
7. Limitations of The Study
This study has some limitations. First, the study was conducted in a single private Historically Black College and University with smaller sample size which diminishes the generalization power of the study. This study conducted among students who came from different schools with unknown previous impact of burnout, therefore a longitudinal assessment of these students would be a more appropriate approach. Further, the lack of a group of non-medical students as a control and the lack of participation of other students is also a limiting factor and it impacts overall results of the survey.
8. Conclusion
In summary, medical student burnout is common, and additional more effort should be made to study its prevalence amongst medical students, its racial and socioeconomic effects, and subsequent training that will effectively address the emotional, mental, and physical challenges inherent to medical school. Given that burnout has been significantly associated with suboptimal patient care, interventions that improve medical student mental health, and subsequently physician mental health, have the potential to improve the quality of healthcare and patient outcomes in the long term.
Competing Interests
The authors declare that they have no competing interests.