1. Introduction
Although engagement in productive activity or employment was the key factor in sustaining recovery for people with schizophrenia, Rosenheck et al. [1] stated that over 70% of the sampling subjects in their study were reported with no employment activity. Importance of neuro-cognitive functions and social functioning in sustaining supported employment among adults with severe mental illness (SMI) were reflected in a local study [2]. Deficiency in their productive living could lead to an enormous demand on social welfare and health maintenance. To understand the difficulties of the persons with schizophrenia especially in coping with productive work, investigations on neurocognitive functioning were often under the researchers’ spotlights. Some of the studies even regarded neurocognitive impairmentas the core of the disorder [3] and was able to provide consistent explanation to functional impairments among people with schizophrenia [4].
Social cognition, which reflected one’s ability in constructing mental representation about self and others [5], demonstrated stronger correlation with community functioning in comparing to neurocognitive functioning [6]. And it offered a unique perspective to quantify interpersonal difficulties in people with schizophrenia [7]. According to Lysaker et al. [8], the construct of social cognition consisted of four major components, including affect recognition, theory-of-mind, emotional intelligent and attribution style. Deficits in social cognition could be described as a divergence between actual and perceived social signal, which led to misunderstanding in social situations [9].
Studies on cognitive profiles of people with schizophrenia had indicated that speed of processing; together with social cognition best distinguished this group of individuals from a community sampling [10]. However, the relationship between neuro-cognition and social cognition remained debatable. Van Hooren et al. [11] conceptualized the deficits of social cognition and neuro-cognition in two separated pathways, named the “affective pathway” and “neurocognitive pathway” respectively, while the affective pathway accounted for their hypersensitivity in social situations and the neurocognitive pathway reflected structural deficits and other chronic courses of the disorder. Bell, Tsang, Greig and Bryson [12] had demonstrated how social cognition mediated the effect of neuro-cognition on community functioning in a three-factor model, proposing that impairment in neuro-cognition could lead to more problems with social cognition.
The purpose of this study aimed to document the first profile of the neuro-cognition and social cognition for a local sample of people with schizophrenia and explore the correlation among the two areas. We hope the results would facilitate further research in this area and fill the knowledge gap in local evidence.
2. Objective
- To review the neurocognitive and social cognitive profiles of people with schizophrenia in a local rehabilitation setting
- To investigate the correlation between neuro-cognition and social cognition of people with schizophrenia or related illnesses.
3. Methodology
This is a prospective cohort analysis of patients admitted consecutively to occupational therapy services in a local hospital for mental health. Single point assessment performed by the case therapist with standardized tools on recording the neuro-cognitive and social cognitive states was performed, in addition to demographic and medical information.
3.1 Measure
Matrics Consensus Cognitive Battery (MCCB) was used in this study as the standard measure for neuro-cognitive functions, including social cognition. It is a standardized battery, tailoring for adults with schizophrenia and related illnesses. MCCB was a popular assessment tool among studies on schizophrenia [13,14] and it also demonstrated good test-retest reliability in researches among Chinese population [15]. MCCB included ten tests that measure seven cognitive domains, including: speed of processing, attention, working memory, verbal learning, visual learning, problem solving & reasoning and social cognition. In order to create a common metrics between different tests, a standardization and co-norming process was conducted by Shi and colleagues [15] among 656 healthy volunteers in China. Domain scores were calculated by the MCCB computerscoring program and presented in term of T-score and percentile so as to facilitate the interpretation of test result in clinical practices. The usual administration time of MCCB was around one to one and a half hours. Case therapists were trained as rater using MCCB.
3.2 Subjects
A cohort of individuals with an ICD-10 diagnosis of psychosis, schizophrenia or schizoaffective disorder referred for occupational therapy services during the period from February of 2015 to August of 2015 was recruited. All subjects were admitted to adult psychiatric wards with age limited from eighteen to sixty-five. People with neurological disorders or primary diagnosis of substance abuse were excluded. All assessments were conducted after the individuals were mentally stable.
3.3 Data analysis
Descriptive statistics were performed on demographic data. In consideration of the significant effects from age, gender and education on normative data [15], we adopted the packaged computation “Age, gender and education corrected” of MCCB for calculation in order to minimize the influences from demographic variances. Kendall rank correlations were performed for correlation analysis across the seven domain T-scores in MCCB in view of the small sampling size. Statistical package for the social science (SPSS) version 22 was used.
4. Result
4.1 Demographics
Forty-four subjects completed the data collection. Thirty-three (75%) of them were diagnosed with schizophrenia, eight of them with paranoid schizophrenia and three of them with other psychotic disorders, including psychosis and simple type schizophrenia. Average sample age is 39.36 (M= 39.36, S.D. = 13.26). Twenty-two (50%) of them were female. Their average years of education were 11.84 (M = 11.84, SD = 3.29).The average years of onset were 9.43 years (M = 9.43, SD = 10.75) and the number of previous psychiatric admissions in average was 2.86 (M = 2.86, SD = 4.23).
4.2 Profile of neuro-cognition and social cognition
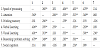
For the 44 subjects, with age, gender and education corrected, the mean T-scores of MCCB domain tests presented in Table 1, indicated the presence of impairments (below one standard deviation from mean T-score) across six domains in MCCB, except “Working memory”(M = 47.29, SD = 12.34). The domain scores of “Social cognition” (M= 30.18, SD = 11.07), “Verbal learning” (M = 38.70, SD = 8.46) and “Speed of processing” (M = 35.09, SD = 14.34) were the three most poorly performed cognitive domains.
In this study, MCCB was firstly presented with documented results for persons with schizophrenia from a local hospital. It was regarded as a reliable tool from the results shown in our sample, with Cronbach’s Alpha of 0.787 across 7 domain items. Inter-item correlation distinguished ‘social cognition’ from others which specifically poor from 0.075 in “social cognition vs attention”, 0.095 in “social cognition vs working memory” and 0.099 in “social cognition vs reasoning / problem solving”; while other items ranges from 0.230 to 0.617. Cochrane’s Test for Between-items Means Square of whole MCCB was 59.746 (p<0.001).
The result of Kendall rank correlation test showed similar findings with significant correlations (p<0.05) shown among all the domain scores except social cognition. ‘Social cognition’ was only correlated with the domain score of ‘Visual learning’ (r (44) = 0.363, p <0.05) (Table 2, Figure 1).
5. Discussion
This is the first local series on the cognitive profiles of people with schizophrenia, using Matrics Consensus Cognitive Battery (MCCB) as a measurement tool and was found reliable. The results showed that neurocognitive deficits were common among the subjects with schizophrenia in our study, particularly on social cognition, verbal learning and speed of processing. The study of Kern et al. [10] on 176 people with schizophrenia or schizoaffective disorder by MCCB had stated that speed of processing; working memory and social cognition were the three most impaired domains, which echoed with our findings. Concerning about the impairment of speed of processing across multiple studies, Knowles, David and Reichenberg [16] had stated that it could be the largest single cognitive impairment in schizophrenia, while Bachman et al. [17] suggested that neurological vulnerability, failure to utilize relational memory and dosage of particular antipsychotic medication account for this impairment. Beside, McCleery et al. [18] stated that functioning of working memory and social cognition were relatively preserved among people with first episode schizophrenia when compared to people with chronic schizophrenia. Thus, it was not surprised that our current sample, a relatively advanced illness profile (Year of onset, M = 9.43, SD= 10.75)demonstrated a declining performance in social cognition along the progression of disorder.
Unlike other neurocognitive domains which are inter-correlated in a significant manner, social cognition was only correlated significantly with visual learning (r (44) = .363, p<.05). Social cognition, under the construct of MCCB, might reflect different characteristics than the remaining neuro-cognitive areas. The results of correlational analysis of our study was similar to the idea suggested by Van Hooren et al. [11] that neuro-cognition and social cognition were nonoverlapping areas of vulnerability in people with psychosis. Evidence on correlation between social cognition and visual learning was still limited, although it had been proved that one’s gaze cueing and visual attention could influence on perception of others [19]. Further research on the relationship among these two areas may shed light on design of interventions for persons with schizophrenia in enhancing their productive activities in social context.
6. Limitation
Small sample size was the obvious limitation of this project, which restricted our choice in statistical analysis and generalization. The wide age range of subjects also raised our concern, as aging was a crucial factor, leading to changes in neurocognitive functioning [20]. The social cognitive domain of MCCB was measured by Mayer- Salovey-Caruso Emotional Intelligence Test (MSCEIT), focused on measurement on emotional intelligence. The properties of affect recognition, theory of mind and attribution style in social cognition remained unexamined, which also limited our choice in correlational testing. Finally, previous studies had suggested that correlational analysis between neuro-cognition and social cognition often completed in a three factors model. Without capturing the severity of symptoms of the subjects, our opportunity to examine how one’s mental condition moderates social cognitive and neurocognitive performances was limited.
7. Conclusion
This study has demonstrated that impairment in social cognition was common among people with schizophrenia. However, the correlation between neuro-cognition and social cognition remained debatable. It was postulated that the inclusion of symptomatic or subjective measurement in social situation might help to clarify the linkage between these two constructs. Besides, detailed investigation on constructing components of social cognition could open more opportunity for correlation analysis study in future.
Competing Interests
The authors declare that they have no competing interests.