1. Background
Multiple studies of long-acting injectable (LAI) antipsychotic medications for schizophrenia have demonstrated superior clinical outcomes when compared to intermittent dosing [1-3]. Unfortunately, these studies have been confined to patients with normal organ function. Patients with schizophrenia are three times as likely to have comorbid renal impairment, and four times as likely to have comorbid liver disease as compared to patients without schizophrenia [4,5]. The control of chronic medical conditions in patients with schizophrenia is confounded by poor insight, engagement, and access to care, particularly in the context of uncontrolled psychotic symptoms [6]. Additional data on the use of LAI antipsychotics in patients with renal dysfunction may lead to improvements in medication adherence and both medical and psychiatric disease control [7]. Clinician apprehension to use such agents in these patients may contribute to long periods of suboptimal disease control. We describe a case that illustrates this problem.
2. Case Report
The patient is a 63-year old man with a history of schizoaffective disorder and end-stage renal disease (ESRD) secondary to type 2 diabetes mellitus and hypertension chronically managed with thrice weekly hemodialysis. He presented to the study center with acute onset of hyper-religious delusions, disorganized thought and speech, and violent behavior. Workup at this time was unrevealing for toxic, metabolic, endocrine, or neurological cause of his symptoms. His outpatient regimen consisted of quetiapine 400 mg daily and sertraline 100 mg daily, but at the time it was unclear if he had been taking any medications. These agents were continued, and olanzapine 10 mg twice daily was added with rapid improvement of his symptoms, suggesting outpatient medication non-adherence. He was discharged to home shortly thereafter.
Approximately 48 hours later, he called the police on himself, and was again noted to be making hyper-religious and disorganized statements. When police arrived at his residence he was combative and frankly psychotic, and thus was brought to the study center again for safety and stabilization. Corroboration with the patient’s family revealed that he had been taking no medications since discharge. At this time an extensive review of his previous psychiatric history was conducted. His family reported a very large number of hospitalizations for psychiatric complaints since his 20’s. The patient’s longest documented period without symptoms resulting in hospital admission was 14 months after review of a six year period. Medication non-adherence was felt to be a significant contributor to the patient’s frequent admissions. Due to this, and due to rapid improvement in psychotic symptoms while receiving antipsychotic medications in a supervised setting, we sought to initiate LAI psychotic therapy. Due to the patient’s ESRD, an extensive literature search was conducted, and the patient was ultimately administered 100 mg of risperidone microspheres by intramuscular injection with concurrent oral risperidone (4 mg nightly). This dose was selected because in the past the patient had required 8 mg of oral risperidone daily for symptom control, a dose which he tolerated. This daily oral dose roughly equates to 100 mg of the long acting product [8]. Additionally, adverse effects associated with LAI first generation antipsychotics were considered unacceptable in this patient. Plans were made for monitoring of antipsychotic plasma concentrations. The patient remained in hospital for an additional 2 weeks due to care coordination issues. During this time he displayed marked, sustained improvement in his psychotic symptoms. On examination he had no evidence of somnolence, orthostasis, extrapyramidal symptoms, gynecomastia, or galactorrhea. An Abnormal Involuntary Movement Scale was conducted and rated as 0. Eventually he was discharged to a personal care home, with excellent symptom control at the time of discharge.
2.1 Therapeutic drug monitoring
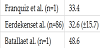
The patient received a 100 mg intramuscular injection of risperidone microspheres. During the first 3 weeks following this injection, he also received 4 mg of oral risperidone daily. Blood samples were taken at 1 hour post-dialysis on day 7 after initial administration of LAI risperidone with oral bridge. Sampling occurred approximately 12 hours after last administration of oral risperidone. The patient received intermitted hemodialysis via an upper extremity arteriovenous graft using a Revaclear© 300 high flux dialyzer at an ultrafiltration rate of 9.1 milliliters, kilogram-1, hour-1 for a total ultrafiltration volume of 2.5 liters (blood flow rate: 400 milliliters, minute-1, dialysate flow rate: 800 milliliters, minute-1). Total concentrations of risperidone and 9-hydroxy-risperidone were analyzed from plasma using quantitative liquid chromatography-tandem mass spectrometry, which was conducted by a commercial laboratory. Post-dialysis day-7 plasma risperidone and 9-hydroxy-risperidone concentrations were <5.0 ng/ mL and 33.4 ng/mL, respectively (Table 1).
All procedures performed were in accordance with the ethical standards of the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research and the 1964 Helsinki declaration and its later amendments. Informed consent for the publication of medical data and treatment procedures was obtained from the patient. The need for Institutional Review Board approval was waived due to the all study procedures being performed as a part of routine patient care.
3. Discussion
Risperidone is a benzisoxazole containing antipsychotic that was discovered in 1986 after a decade of searching for compounds capable of antagonizing the behavioral effects of the hallucinogen lysergic acid diethylamide (LSD) [9]. It is a potent antagonist of dopamine-2 receptors, serotonin-2A receptors, and others [10]. Immediate release risperidone has adequate oral bioavailability (70%), extensive tissue distribution (1-2 L/kg), requires hepatic metabolism for activation via cytochrome P450 2D6 isoforms, and its active metabolites are in large part renally eliminated [11]. In addition, cytochrome P450 3A4 contributes significantly to risperidone metabolism [12,13]. Risperidone has a 21-hour half-life and oral formulations have been shown to accumulate by as much as 60% above usual therapeutic plasma concentrations in patients with severe renal disease [11]. Risperidone is also available in a long acting intramuscular injection (LAI) which utilizes a polymer matrix [14]. This vehicle consists of successive ester linkages that are slowly hydrolyzed in aqueous environments over a period of 2 months [15]. This results in a 6 day half-life, with LAI risperidone being administered every 2 weeks at doses of 12.5 mg, 25 mg, or 50 mg [14].
Because of its slow release and resultant long half-life, injection of LAI risperidone is not expected to produce steady state plasma concentrations for at least 3 weeks, with some reports suggesting steady state is not reached for 6 weeks [16]. Because of this long “ontime”, oral risperidone is used concurrently during the first 3 weeks of therapy [14]. Published data [8] are available on the time course of plasma concentrations achieved throughout the early titration period when LAI risperidone is being bridged with oral risperidone. This is precisely the time period during which our patient had plasma risperidone concentrations measured (day 7). Because the aforementioned data [8] come from patients with normal renal function, we wanted to compare accumulation in our patient to accumulation observed in the subjects of this study.
In the most definitive analysis of the pharmacokinetics of LAI risperidone, Eerdekens and colleagues conducted an open-label trial [8] in which 86 patients with schizophrenia received LAI risperidone at doses of 25, 50, and 75 mg biweekly. LAI risperidone was initially bridged with 4 weeks of oral risperidone at doses of 2, 4, or 6 mg daily. In the 75 mg intramuscular-6 mg oral group (which most closely approximates our patient’s dosing of 100 mg intramuscular-4 mg oral) they observed a mean day-7, end-dose interval, combined risperidone and 9-hydroxy-risperidone concentration of 32.6 (±15.7) ng/mL. Steady state plasma concentrations for this dose ranged from 32.6- 80.6. (Figure 1, adapted with permission from Eerdekens et al.). The corresponding plasma concentration in our patient fell somewhere between 33.4-38.4 ng/mL (Table 1). Thus, early accumulation of risperidone in our patient was well below that of patients with normal renal function who had the greatest amount of accumulation in the Eerdekens trial, and reasonably close to average accumulation observed in this well performed study.
Only one additional case report exists documenting the use of LAI risperidone in a patient with ESRD [17]. In this patient receiving 50 mg of LAI risperidone bridged with 6 mg of oral risperidone, day 7 post-dialysis combined plasma risperidone concentration was 48.6 ng/mL. Consistent with our experience, this case also demonstrated that early LAI risperidone accumulation in a patient with ESRD is at most at the upper limit of that observed in subjects with normal renal function [17,8]. This case also reported no major adverse effects and adequate control of psychosis.
Clearly these data have significant limitations. Case reports are subject to significant observer bias, and contain no control group with which to make comparisons. For this reason we relied on pharmacokinetic data published in another study, however this analysis strategy itself poses issues as similar study procedures cannot be achieved in the course of usual patient care. We draw attention to a large pharmacokinetic trial that used LAI risperidone at a dose of 75 mg, while in the case of this patient we used 100 mg. Thus, direct comparison of drug accumulation cannot be reliably assumed. In addition, our data focus on drug exposure early in the course of accumulation, as we were acting out of an abundance of caution. To firmly establish that this dose is safe, we would need to wait for future concentrations measured after repeated injections more than 6 weeks. Unfortunately, following this hospitalization the patient transferred care to another hospital system due to insurance issues, and thus it was not possible to obtain additional plasma concentrations. Given that prior to this report, only a single instance of LAI risperidone use in ESRD had been published, our primary intention was to report our findings on the presence or absence of early over-accumulation or adverse effects. However, an understanding of long-term drug exposure is of paramount importance in this clinical situation.
4. Conclusion
There is an almost complete lack of data describing the use of longacting formulations of antipsychotic medications for patients with schizophrenia and ESRD. However, this strategy can be successful, as demonstrated in this case report. If used, clinicians should monitor antipsychotic plasma concentrations periodically and closely monitor for emergence of toxicity.
Competing Interests
The authors declare that they have no competing interests.
Author Contributions
MJF: project conception and design, data acquisition and analysis, manuscript preparation, final approval, YY: project conception and design, data analysis, manuscript preparation, RC: project design, manuscript preparation, final approval.