1. Introduction
The inflammatory bowel diseases (IBD), including ulcerative colitis, Crohn disease and IBD-undefined, are chronic inflammatory disorders of the gastrointestinal tract most often diagnosed in adolescence and young adulthood [1]. IBD often presents with intestinal symptoms, including abdominal pain, blood loss, and diarrhea, but can also be associated with systemic symptoms of weight loss, joint and skin changes, and psychological comorbidities, including depression and anxiety [2]. Although the etiology of IBD remains largely unknown, it involves a complex interaction between the genetic, environmental or microbial factors and the immune responses [3].
Approximately 25% of patients with IBD present before age 20 years. Among children with IBD, 4% present before age 5 years and 18% before age 10 years, with the peak onset in adolescence. The incidence of pediatric IBD is approximately 10 per 100 000 children in the United States and Canada and is rising [1]. Studies in developing countries in South America, Africa and Asia have also shown a significant increase in IBD [4]. Although the incidence and prevalence in Chile is still unknown, one study has suggested an increase in these diseases approaching the levels reported in developed countries [5]. However, these data refers only to adult patients and actual data in pediatrics is still unknown.
Regardless the statistics, recognizing and addressing care gaps plays a critical role in optimizing disease outcomes in pediatric IBD. Medication nonadherence is common in chronic pathologies and is associated with poor outcomes. While this disease requires longterm medication usage to maintain remission, nonadherence is common and adversely associated with poorer clinical outcomes [6]. Nonadherence affects at least 1 in every 6 patients and its repercussions are of clinical relevance, such as hospitalizations or visits to the emergency department. In addition, it has been found that age is a factor that is related to lack of adherence, as is the case of adolescents [7].
All of the above ratifies the need for comprehensive and multidisciplinary care of patients with IBD. From the pharmacists’ point of view, individualized plan of care can be proposed, monitoring the pharmacotherapy and its outcomes in each patient. Pharmaceutical care is the “responsible provision of drug therapy for the purpose of achieving definite outcomes that improve a patient’s quality of life” [8]. In this context, the pharmacotherapy follow-up is a structured process in which pharmacists are held accountable for the patients’ needs related to specific drugs for taking clinical decisions in an effort to achieve the expected outcomes in health [9]. After identifying drug related problems, pharmaceutical interventions are proposed. These actions are planned, documented and conducted involving patients, caregivers and professionals, aiming to solve or prevent problems that interfere or may interfere in drug therapy, being an integral part of the pharmacotherapy follow-up process [10].
An action guide for the community pharmacist in IBD was developed in Spain but the target population was adults [11]. So far, no publications were found related to the involvement of pharmacists with IBD pediatric patients. Therefore, in this paper our purpose is to describe a pharmacotherapy follow-up to pediatric outpatients with inflammatory bowel disease.
2. Materials and Methods
The pharmacotherapy follow-up was conducted at pediatric Hospital Exequiel González Cortés (HEGC), in Santiago (Chile), from April to September 2018. To receive the service we invited pediatric outpatients, and their caregivers, attended at the HEGC diagnosed of IBD and with, at least, one control in the last six months. All patients had to obtain their medications from the Hospital's Outpatient Pharmacy. Additionally, the caregivers must accept participation in the study by signing an informed consent.
Two pharmacists carried out the follow-up through monthly interviews with the patients and their caregivers. Prior to admission to the first interview, each medical chart was reviewed. In first interview, data of each medical condition and history of allergy was recorded along with the pharmacotherapy used by the children.
Patients and caregivers were asked in relation to pharmacotherapy expectations and concerns, life habits and periodicity of medical checks. Finally, an open question was attached about additional discomforts.
Data related to anthropometric measurements, laboratory parameters and colonoscopy was registered. Also, Pediatric Ulcerative Colitis Activity Index (PUCAI) [12]; Visual Analogue Scale (VAS) [13] and the Simplified Medication Adherence Questionnaire (SMAQ) [14] adherence tests were applied.
With all this information, drug related problems (DRP) were identified and the appropriate interventions were proposed to solve them. The interventions were addressed to the patients and caregivers or to the health team. For the purposes of this report, the DRPs were classified according to Cipolle and Strand [15].
During all the process, the pharmacists provided support material to the patients, such as devices to cut and store tablets and educational leaflets designed by the pharmacy team.
In order to know the perception of the pharmaceutical care received and the resolution of problems a self-administered questionnaire was applied to caregivers. The survey had ten questions related to the perception of the utility and quality of the care received. Caregivers must punctuate the questions with a Likert scale and an open space for comments. Before its application, a team of pharmacists reviewed the survey to ensure its face validity.
Data was tabulated using Excel software for conducting the analysis of the results. Numerical variables were described as means and standard deviations, and categorical variables as proportions.
The Ethics Committee of the Southern Metropolitan Service in Santiago authorized the project. In addition, for the inclusion of patients to the project, informed consent was required for the caregivers, and informed assent was asked to the pediatric patients who attended the interviews. To avoid individualizing patients, all the data was coded and grouped in Tables.
3. Results and Discussion
Of the total number of patients treated in the HEGC with IBD (n: 21), 20 were eligible for pharmacotherapy follow-up and 12 accepted the service. All the patients assisted, at least, to a three appointments with the pharmacists.
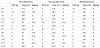
The sociodemographic characteristics of patients and caregivers are in Table 1. As the HEGC is a public hospital, all patients had state health coverage. Moreover, in 90% of the cases, the caregiver is similar in gender to other publications [16], where the woman is who provides continuous care [17]. Parents of children with chronic illness are primary nurturers in their children’s lives and key members of their children’s health care teams. They can experience increased caregiver challenges including augmented medical related costs, challenges with childcare, and constrained employment opportunities [18].
The 12 patients had ulcerative colitis (UC) and most of them were teenagers. The number of male patients were predominant however; studies show there are no differences in sex for UC [19,20].
Additionally, 19 comorbidities were registered, where five patients were overweight, five had acne, two had obstructive bronchitis and two suffered obesity, among others.
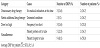
The data related to ulcerative colitis activity and adherence obtained during the follow-up is described in Table 2. According to SMAQ, five patients were non-adherents at the beginning of the follow-up while all were adherents in the third interview. The PUCAI scale indicated that all the patients were in remission.
3.1 Pharmacotherapy and drug related problems
All patients used 35 drugs in total, with an average of 2.9 + 1.3 drugs per patient. These medications include IBD therapy, auxiliary pharmacotherapy, and drugs necessary to treat other comorbidities.
The twelve patients used oral mesalamine as their basic therapy. This drug remains the first-line drug for mild-to-moderate UC [21]. Of these, six patients used only mesalamine and the others used mesalamine in combination with azathioprine. The doses of azathioprine were in range according to clinical guidelines.
Regarding to mesalamine doses, a range from 20 to 90 mg/kg/ day was found; while clinical guidelines suggest dosing for oral mesalamine from 60 to 80 mg/kg/day to 4.8 g daily [22]. No patient received doses higher than those recommended in literature did.
The frequency of mesalamine administration was twice (b.i.d.); three (t.i.d.) and four (q.i.d.) times a day. In two of the three patients who used mesalamine q.i.d., the physician accepted to change their frequency in order to simplify the treatment and adjust it to the recommendations of the clinical guidelines [23].
Zheng X et al. conducted a meta-analysis to evaluate the efficacy and safety between once daily and b.i.d. regime dosing of mesalazine for mild-to-moderate UC. They concluded that both regimes were effective and safe [21]. However, in our follow-up, it was not suggested to change the dose scheme to a once daily dose since the published studies were developed in adults and there was a lack of data to validate its use in the pediatric population.
The auxiliary pharmacotherapy for IBD consisted of vitamins and mineral supplements such as folic acid of 1mg and 5mg, cholecalciferol 2000 IU and calcium carbonate of 320 and 450mg. In addition, hydrocortisone was prescribed as withdrawal regimen for corticosteroids used to induce remission, or as a treatment for adrenal insufficiency due to its prolonged use.
During the follow up, 22 DRP were identified (Table 3). Mesalazine and azathioprine were the drugs responsible for fifteen (68%) problems. Other drugs involved in one DRP each were hydrocortisone, folic acid, cetirizine, omeprazole, trimebutine and sucralfate.
With regard to the DRP, nonadherence was the main problem identified; this data agree with the claims that suboptimal adherence to medication is common in patients with chronic diseases [24]. Additionally, rates of adherence to medication regimens among children with chronic diseases are similar to those among adults with chronic diseases, averaging about 50 percent, with decrements in adherence occurring with time [25].
In the case of IBD, efficacy is dependent upon adherence to medication regimens, which has been reported to be only 40-60%, by self-report and urinary drug measurements, in patients prescribed mesalamine. These self-report may even underestimate the extent of nonadherence, as self-reporting typically overestimates an individual’s adherence [26].
3.2 Pharmacists’ interventions
Thirty-five interventions were proposed, nineteen to the patients or caregivers and the remaining sixteen were directed to the health team. The interventions to the patients were the educational type in order to reinforce adherence to long-term treatments. In eight cases, the patients received devices to cut and store the medicines.
Interventions to the health team were suggestions to change the frequency of administration; to change the treatment scheme (number of tablets in one shot); to finish one treatment or add a new medication to the therapy; and suggest the visit to another health professional. From these sixteen interventions, 12 were accepted. Rejected suggestions were related to the change of the therapeutic scheme and the consulting to a different health worker. The rate of rejected interventions correlates with a Spanish study, where 27% of the pharmacists suggestions were rejected [27].
After the third interview, 20 DRP were solved of the 22 identified. The fourteen problems related to non-adherence were addressed and resolved.
During the follow-up different problems were identified, but there were not related to pharmacotherapy. Those arose from reviewing medical charts or, in the interviews, patients or caregivers expressed them. These problems were associated to health outcomes and patient quality of life. At this point, it is necessary to emphasize the concept of integral care, which focuses on the medication, but also focuses on the individual and their continuing health needs and medical conditions [28].
Regarding to the satisfaction questionnaire, the responses of the 12 caregivers related to the quality of the pharmacist consultation were between "good" and "very good", which reflects complacency with the care received.
Among the limitations, it should be noted the small number of patients in the follow-up process. This circumstance does not allow extrapolate the results to other groups with IBD, however, considering the total hospital population with IBD eligible for follow-up (n = 20), it reflects a recruitment greater than 50%.
Furthermore, the team of the Gastroenterology Service did not meet periodically. Gastroenterologist, nurse, pharmacist, social worker, psychologist and nutritionist formed the team and the absence of meetings made communication and decision making difficult for the interventions.
4. Conclusion
During six months the pharmacotherapy of twelve pediatric patients with IBD was optimized, this was done through the pharmacotherapy follow-up, identifying twenty-two DRP, which were addressed with interventions to patients and the health team. Twenty problems were resolved and most of the suggestions were accepted. The caregivers expressed their satisfaction with the pharmacist intervention to optimize the children pharmacotherapy.
Therefore, for this group of patients, a continued pharmaceutical care over time is recommended, focused on the adherence to pharmacological treatment and other health problems that may be manifested, either referred by the patient or caregiver, or investigated through laboratory exams. In this way, the patient would have a comprehensive care provided by a multidisciplinary team of health professionals.
Competing Interests
The authors declare that they have no competing interests.
Author Contributions
JBV and JCE made substantial contributions to the conception
and design, the acquisition of data, the analysis and interpretation of
data. In addition, both revised critically the manuscript and gave final
approval of this version.
ACL made substantial contributions to the conception and the study
design; also analyzed the data and interpreted it. In addition, revised
critically the manuscript and gave final approval of this version.
EMV made substantial contributions to the conception and design,
the analysis and interpretation of data. In addition, was involved
in drafting the manuscript and reviewing it critically on important
intellectual contents and gave the final approval of this version.