1. Introduction
The sensation of burning discomfort or pain behind the breastbone is a frequently experienced disorder [1]. These types of symptoms are often related to gastro esophageal reflux disease (GERD), pregnancy or cardiac disease [1]. GERD may develop when prolonged exposure of the lower esophageal mucosa to gastric acid with a pH < 4 occurs more than one hour per day. The corresponding symptom is frequently referred to as “heartburn.” The increased exposure to gastric acid may lead to a breakdown of the mucosal defence mechanisms, resulting in inflammation, erosions, and ulcerations, ultimately and scarring fibrosis of the distal oesophagus [2].
For many years, antacids were the treatment of choice related to GERD and peptic ulcers. These treatments are frequently combined with anticholinergic agents to reduce the output of gastric acid. The main disadvantage with antacid treatment is the need for repeated dosages during the day to relieve symptoms. The first breakthrough for pharmacological treatment came with the introduction of histamine 2(H2) receptor antagonists in the 1970s [3]. The second occurred with proton pump inhibitors (PPI) twenty years later. PPIs are now the gold standard in the treatment of GERD. However, medical therapy is not curative and requires continuous treatment [1].
In 1955, Rudolph Nissen performed “gastro plication”, later denoted as fundoplication(4). Surgery is an effective and curative approach. Several minimally invasive operative methods have acceptable merits; however, the disadvantages include the risk for severe side effects, complications and the irreversibility of the procedures.
Is it possible to develop a treatment procedure, addressing some of the possible reasons for the disease? The role of osteopathy in understanding and treating the musculoskeletal system has been known for over a hundred years [5]. During the last decades, this understanding has greatly changed by integrating techniques, such as the cranio-sacral and the visceral systems [6,7].
One possible reason accounting for the development of GERD might be an insufficient closing of the lower esophageal sphincter (LES) [1]. The effect of Osteopathic Manual Therapy (OMT) of LES has previously been described [8]. The objective of this study was to compare pressure values in the examination of esophageal manometry of the LES before and immediately after osteopathic intervention in the diaphragm muscle. Thirty-eight patients with GERD randomly allocated to OMT or sham technique.The average respiratory pressure (ARP) and the maximum expiratory pressure (MEP) of LES measured by manometry before and after OMT at the point of highest pressure. Significant difference in favor of OMT detected on ARP,but not on MEP. The study demonstrated a positive increment of OMT in the LES region soon after its performance. The OMT described consisted only of diaphragm stretching using breading techniques. However, OMT includes several techniques that might influence LES and increasing the effect on the sphincter. It might be possible to use the visceral techniques to stimulate the closing mechanism via the crural diaphragm (9). In order to describe an OMT procedure in treatment of GERD, a set of OMT techniques has to be combined and investigated concerning the effect on the GERD symptoms.
2. Materials and Methods
2.1 Populations and subjects
The reference population consisted of patients of both gender suffering GERD defined asgastroesophageal reflux, without erosive disease and known effect of anti-reflux medication.
The study population consisted of patients passed the age of 18 years and suffering from GERD withouthiatus hernia ≥ 5 cm, cancer and uncontrolled bacterial, viral, fungal or parasite infection.The patients had to have at least one of the five following symptoms: heartburn, retrosternal pain, acid in the mouth, epigastric pain and tension and pain in the lower thoracic spine. Pregnant and breastfeeding women and patientpreviously undergone surgery of the upper abdominal tract were excluded. In order to avoid erroneously inclusion, endoscopic investigation of the upper gastrointestinal tract was performby the Department of Gastroenterology at Hammerfest Hospital.
Forty endoscopically investigated GERD patients,recruited by local general practitioners (GPs) voluntarily received treatment at the Osteopathic Clinic in Alta, Norway. Of these patients, 18 did not fulfil the criteria for inclusion or met the exclusion criteria.
The remaining 22 patients gave written consent for participation. The study sample consisted of 18 female and four male patients. The mean age and duration of symptoms were 47.4 years (range: 22-72) and 20.4 months (range: 3-36), respectively. During the study, five patients used antacids, two H2 receptor antagonists and one used PPI. The remaining 14 patients did not use concomitant GERD medication.
2.2 Study design
The study was performed as a retrospective, single-centre and onearmed interventional trial using the patients as their own control.
2.3 Osteopathic treatment
The osteopathic treatment combined the four techniques: traction of the cardia, mobilisation of the diaphragm and thoracic spine and posture correction.
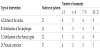
Between three and 12 osteopathic treatments were given by the same therapist. All of the included patients were treated via the musculoskeletal and the fascial system and given both diaphragm mobilisation and traction of the cardia (Table 1).
2.3.1 Traction of the cardia
The ligament of Treitz is a structural connection with contractile fibres (Figure 1) between the right crus of the diaphragm and the duojejunal junction. These crura surround the LES and increased tension might be a part of the closing mechanism (9, 10). This technique should be repeated three times and supports the complete closing of the LES.
Procedure:
- The patient is lying in a supine position on the table. The operator is standing on the left side, at the level of the thorax, facing the patient’s feet.
- The operator’s left hand stabilises the patient’s vertebral column at the level of the 10th thoracic vertebrae.
- The operator’s right hand grasps the patient’s epigastric tissue with an open palm.
- A longitudinal stretch is performed on this tissue while the patient is inhaling.
- While exhaling, the operator’s hand slowly stretches the tissue in the caudal direction.
- At the end of exhaling, the operator’s hand remains in this position.
- When the patient resumes inhaling, the operator keeps his hand in this position.
This procedure increases tension in the epigastric tissue and the ligament of Treitz and completes the closure of the LES.
2.3.2 Mobilisation of the diaphragm
The patient is placed in a supine position, and the operator stands at the head or at the side of the table. The margins of the lower rib cage are gently grasped and pulled and pushed to its rotation restriction and held as the patient deeply breathes in and out. Sometimes, a superior or inferior vector is added to the direct rotation of the thoracic cage so there is a palpable movement of both sides of the diaphragm during deep breathing, i.e., both leaves of the diaphragm move well. The position is held for approximately three large breaths so that the fascial preference is eliminated and the respiratory effort has redomed the diaphragm [11].
2.3.3 Mobilisation of the thoracic spine
- Both the left and right crura surround the LES, and their contractions are important for closure (9). These crura are the muscular connection between the body and the transverse of the second lumbar vertebra. Contractions of these muscle fibres support the closing mechanism of the LES. The following technique must be repeated three times.
- The patient is lying on the left side with the operator standing on the right side, facing the back of the patient.
- The left hypothenar is placed on the patient’s sternum, and the right palm on the spine, at the level of the 10th thoracic vertebrae. The patient is asked to inhale and then slowly exhale. While exhaling, the operator’s left hypothenar puts pressure on the sternum in a cranio-dorsal direction. The right palm moves along the spine, at the level of the 10th thoracic vertebrae in an anterior direction.
- At the end of exhaling, both of the operator’s hands remain in this position.
- During the following inhale, the operator holds this extended position.
- During the next exhale, the spine is gradually extended and then fixated. At the same time, the sternum is pressed in a craniodorsal direction.
2.3.4 Posture correction
An extended thoracic kyphosis is common among patients suffering from GERD. This position takes tension away from the diaphragm crus and the closing mechanism of the LES [12]. Thoracic kyphosis may disrupt gastric function and stomach acid can enter the oesophagus. By forcing the lowered thoracic kyphosis into extension and activating deep breathing, the tension of both crura will be increased. The technique must be repeated daily and is performed as follows:
- The patient is lying in a supine position on the bed or couch.
- A pillow, medium hard, not too large, is placed under the 8-12th vertebrae, forcing this part of the spine into extension.
- The patient now tries to relax the back while slowly breathing in and out.
- This position and exercise takes approximately 10-15 minutes and should be repeated once a day, especially in the evenings.
2.4 Clinical procedure
Before the start of treatment, the patient posture was recorded as“normal,” “thoracic kyphosis,” “reduced extension” or both “thoracic kyphosis” and “reduced extension.”
A normal thoracic posture is a slight kyphosis, while thoracic kyphosis, in this study, is an extension of the normal anatomical thoracic kyphosis. Reduced extension is the loss of the ability to extend the thoracic spine.
The occurrence of GERD symptoms related to “forward bending,” “lying flat,” and “consumption of orange juice or coffee” was reported by the patients.
The presence of symptoms of heartburn, retrosternal pain, acidin the mouth, epigastric pain and tension and pain in the lower thoracic spine was reported before, at the end of treatment and three month after last treament.
The treatment effect was recorded by the patients on a Fixed-point scale (FPS) with the following 4 classifications: “no effect” = no change in symptoms, “slight effect” =some symptoms disappeared or were reduced, “moderate effect”=periods with no symptoms, “good effect”= relief of the symptoms [13,14]. The patient continuously recorded concomitant GERD medication during the study.
All of the patients were given a special home exercise and four were advised to avoid coffee. OMT continued as long as improvement between the two last treatments obtained. When the relief or absence of symptoms occurred or a maximum of 12 treatments without a sufficient effect, the treatment discontinued. However, the participant continued with the given home exercise. The observation time was 3 months after the last treatment.The included patients gave written consent for participation in the study.
2.5 Statistical methods
The continuously distributed variables and factors are expressed as mean values with standard deviations (SD), 95 % confidence intervals or total range. The 95 % confidence interval for the mean was constructed using the Student procedure [15]. Categorical or discrete distributed variables are expressed in contingency tables with the number of patients or the prevalence with the 95 % confidence interval. The confidence interval for prevalence constructed using the theory of simple binomial sequences [15].
All the tests performed two tailed with a significance level of 5 %. Changes within and comparison between groups with regards to categorical variables were performed by contingency table analysis [16]. For changes within the groups, cross-table analysis was performed by using McNemar’s test [16].
3. Results
3.1 Effect of the treatment
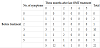
Nineteen patients reported three or more GORD symptoms before the start of treatment (Table 2). After treatment, only one patient reported as many as three symptoms.
The number of GORD symptoms was significantly reduced (p<< 0.01) from before to after the end of the osteopathic treatment. Only two patients reported the same number of symptoms before and after treatment.
The prevalence of heartburn, retrosternal pain, acid in the mouth, epigastric pain and pain in the lower thoracic spine were all significantly reduced (p ≤ 0.004) from before to after the treatment (Table 3). The prevalence of heartburn and retrosternal pain after treatment was found to be 4.6 %. For both variables, the proportion was reduced from 63.6 % to 4.5 %. The proportion of heartburn and retrosternal pain was reduced from 63.6 to 4.6 % (95 % CI: 0.1 – 22.8 %). For acid in the mouth, the proportion was reduced from 44.5 % to 9.1% (95 % CI: 1.1 – 29.2 %) after the end of treatment. The proportion of epigastric pain and pain in lower thoracic spine after the osteopathic treatment was reduced from 95.5 % and 72.7 % to 45 % (95 % CI: 24.4 – 67.8 %) and 40.9 % (95 % CI: 20.7 – 63.7 %), respectively.
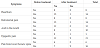
The subjective reported effect was registered as “moderate” or “good” by 77.3 % (95 % CI: 54.6 – 92.2 %) of the patients (Table 4).
Eighteen patients reported forward bending to be the main provocation factor for GERD symptoms while consumption of coffee was reported by 14 patients, “lying flat” by 6 patients and consumption of orange juice by 6 patients. Seven patients reported bending forward and lying flat as the only reasons for GERD provocation, whereas 3 patients reported acid-related reasons. The remaining 12 patients reported both mechanic and acid-related reasons.
Lowered thoracic kyphosis and reduced extension was detected in 19 of the 22 included patients (Table 4). Of these, 78.9 % reported a “moderate” or “good” osteopathic treatment effect.
The reduction in the number of GERD symptoms from before to after treatment was found to be in accordance with the subjective reported effect (Table 4). The patients with lowered thoracic kyphosis and reduced invagination achieved a reduction of at least two GERD symptoms in 78.9 % of the cases during the osteopathic treatment.
3.2 Combined OMT and pharmaceutical treatment
A comparison of the patients receiving only osteopathic treatment with those who received additional pharmaceuticals did not reveal any differences with regard to a reduction in the number of GERD symptoms nor the reported effect (Table 5). The two groups were found to be nearly equal before treatment.
4. Discussion
4.1 Effect of OMT in the treatment of GERD
The total number and the prevalence of all the five GERD symptoms were significantly reduced during the OMT intervention, and the reduction in prevalence was found to be most pronounced for heartburn, retrosternal pain and acid in the mouth. In general, the results from the present study clearly indicate an effect of the included OMT techniques on the five GERD symptoms. However, the main variables are subjective, and the study was performed as an open trial with the patients as their own controls. A large majority of the included patients reported moderate or good effects, which are promising results.
It is reasonable to assume that the obtained effects include a considerable placebo effect. Due to the lack of a control group, the design and the performance in the present study, it is not possible to estimate how much of the obtained effects are caused by placebo. A placebo effect of up to 50 % in the treatment of upper gastrointestinal tract diseases has been reported [17].
It is previously reported one placebo controlled clinical trial of OMT on GERD patients [8]. However , this study did not include the effect on GERD symptoms, but the results from this study actually support present findings. To the best of our knowledge, no controlled clinical studies of OMT in this field have yet been published. To establish and verify the effect of OMT, double blinded placebo controlled studies are needed.
Both the H2 receptor antagonists and PPI reduce the production of gastric acid whereas antacids neutralise the acid. The reason for reflux oesophagitis in general is not obvious. The two main possible reasons is either a ventricle or a LES disorder. When the disease is related to a ventricle dysfunction, pharmaceutical GERD treatment might have both a curative and palliative effect. However, it is well known that discontinuation of the drug treatment results in the relapse of symptoms [1]. This observation indicates that the effect is more palliative than curative. If the cause of reflux oesophagitis is a LES disorder, the commonly used drugs are expected only to have a palliative effect. The mechanism of action for the pharmaceutical treatment of GERD is well documented [18], but what about the OMT techniques used in the study?
The theory behind the chosen techniques is to stimulate and optimise the closing function of the LES. One of the OMT techniques used in the present study was mobilisation of the diaphragm. The diaphragmatic crura curl around the oesophagus as it passes through the hiatus. Flexibility in these structures governs the function of muscular contractions and supports the closing of the LES [9]. The traction of the cardia technique increases the tension in the oesophagus and LES, which also supports tighteningthe closing mechanism [12]. The ligament of Treitz is a structural connection with contractile fibres between the right crus of the diaphragm and the duojejunal junction. The diaphragmatic crura surround the LES, and increased tension is a part of the closing mechanism of the LES. This technique supports the complete closing of the LES [12]. More than 85 % of the patients in the present study were found to have a lowered thoracic kyphosis and reduced extension, demonstrating reduced mobility of the thoracic spine. This effect was mainly observed around the area of Th10 or the level of the LES. The mobilisation of the spine in the direction of invagination will increase the tension of the oesophagus and support the closing ability of the LES. This mobilisation includes the corrected posture which is obtained by straightening the spine.
The esophagus is normally under tension [19]. The function of the closing mechanism of the LES might depend on this tension. Anatomically, this mechanism is described as a sphincter but this description is doubted by several other authors. Leonhardt, Tillmann and Tondury describe the muscular architecture of the lower oesophageal sphincter as “Wringverschluss” [19]. This mechanism only functions when the longitudinal tension of the esophagus is present.
If the tension loosens, the closing of the LES does not complete and acidic fluid can easily enter esophagus. This fact might explain why 18 of the participating patients reported “bending forward” as the main provocation factor for symptoms, such as heartburn, retrosternal pain and acid in the mouth.
The present study demonstrates a significant effect of OMT on GERD symptoms.To what extent will the effects continue after discontinuation of OMT? The available results do not give an answer and must be investigated in future studies.
4.2 Pharmaceutical and osteopathic treatment of GERD
In the present study, eight patients were using pharmaceuticals in addition to receiving OMT. No significant difference between the patients receiving only OMT and those who used additional pharmaceuticals was detected. In the case of differences, the effects favoured OMT alone. However, the number of patients in each group was very small and the results might be additionally influenced by the way the study was performed. Based on the obtained results, one can assume that OMT does not influence the symptomatic effect of H2 receptor antagonists or PPIs. If the results from the present study can be verified in future placebo-controlled and double-blinded studies, OMT could be implemented as an additional treatment for GERD. The pharmaceuticals commonly used today mainly have a palliative effect in the treatment of GERD. By including OMT, a possible curative effect might be added.
5. Conclusion
In conclusion; a combination of the described OMT techniques was observed to have a positive effect in patients suffering from GERD symptoms and may be a promising therapeutic.
Competing Interests
The authors declare that they have no competing interests.