1. Introduction
The treatment of bacterial infections is increasingly complicated by the ability of bacteria to develop resistance to antimicrobial agents often results in treatment failure. WHO has identified that urgent and coordinated action is required at local, national, and international levels to ensure the adequate treatment of patients today and the preservation of the life-saving power of antimicrobials for future generations. With increase in antimicrobial use and misuse, the level and complexity of the resistance mechanisms exhibited by bacterial pathogens have also increase dramatically. Several mechanisms have evolved in bacteria which confer them with antibiotic resistance. These mechanisms can chemically modify the antibiotic, render it inactive through physical removal from the cell, or modify target site so that it is not recognized by the antibiotic [1-3].
Bacterial resistance to antibiotics has been a recognized reality almost since the dawn of the antibiotic era, but only within the past twenty years has the emergence of dangerous, resistant strains occurred with a disturbing regularity. This escalating evolution of resistance coupled with a diminished antibiotic pipeline has led some to claim that a post-antibiotic era is eminent [4]. The annual impact of resistant infections is estimated to be $20 billion in excess health care costs and 8 million additional hospital days in the United States (US) [5,6] and over 1.6€ billion and 2.5 million additional hospital days in the European Union (EU) [7].
S. aureus is a gram positive, facultative anaerobic pathogen with both hospital and community acquired strains. Though traditionally opportunistic, many S. aureus strains are now aggressively pathogenic [8]. It is the most common skin bacterium with 60% of humans being intermittent carriers and 20% being persistent carriers, chronically harboring at least one strain [9].
MRSA is considered to be one of the 18 microbes listed by the CDC as a multidrug-resistant microbe or "superbug" [10]. MRSA is known for causing skin infections in addition to many other types of infections. The majority of MRSA infections are classified as CAMRSA (community acquired) or HA-MRSA (hospital- or health-careacquired) [11]. Statistical data suggest that as many as 19,000 people per year have died from MRSA in the U.S. Data supplied by the CDC in 2011 suggests this number has declined by about 54% from 2005 to 2011, in part, because of prevention practices at hospitals and home care. In addition, hospital deaths from MRSA infection have declined by about 9,000 per year from 2005-2011. However, the CDC recently estimated about 80,000 infections with 11,000 deaths occurred in 2011, but they suggest that a far greater number of minor infections occurred in both the community and in hospitals.
Currently, MRSA bacteria are almost always found to be resistant to multiple antibiotics [11]. All isolated MRSA strains need to have antibiotic susceptibility determined to choose the correct or appropriate antibiotic therapy. Treatment of HA-MRSA frequently involves the use of vancomycin, often in combination with other antibiotics given by IV. CA-MRSA can often be treated on an outpatient basis with specific oral or topical antibiotics, but some serious CA-MRSA infections (for example, pneumonia) often require appropriate antibiotics by IV.
Chitosan, a positively charged polysaccharide biopolymer derived from chitin, exhibits a number of interesting biological properties such as wound healing ability, antimicrobial, and anti-inflammatory activities, and biodegradability [12-14]. Since it was first proposed for antimicrobial activity in 1979 [15], chitosan has drawn attention of many researchers.Chitosan has shown wide spectrum of antimicrobial activity against both gram positive and gram negative bacteria, fungi and yeasts [16-20].
Ethylenediaminetetraacetic acid (EDTA) is a widely known metalchelating agent, substantially used for the treatment of patients who've been poisoned with heavy metal ions together with mercury and lead. The impact of EDTA on bacteria appeared first in 1965 when Brown and Richards stated EDTA as a ‘potentiator’ of the activity of other antimicrobial agents [21]. EDTA has shown to potentiate the actions of other preservatives, antibiotics and cationic surfactants [22-25]. EDTA reversed the antibiotic resistance of tetracycline, penicillin or ampicillin when combined with these antibiotics in strains of Pseudomonas aeruginosa [26,27]. However, the mechanism of antibacterial effectiveness by EDTA is not fully known, it’s chelating ability to bind with divalent cations, deprive the microorganisms of Mg2+, Ca2+, and Fe2+, which are essential factors for microbial growth. EDTA was also shown to enhance destabilization of the S aureous [28]. The use of EDTA in combination with minocycline had shown increased bactericidal effect on antibiotic-resistant S. aureus cells [29].
The aim of this investigation was to evaluate the efficacy of levofloxacin in combinations with chitosan and chitosan-EDTA against both normal strain and resistant strain of SAin both in vitro and in vivo.
2. Material and Methods
Levofloxacin and EDTA were purchased from S. D. Fine Chemical Limited, Mumbai, India. Chitosan (degree of deacetylation ≥ 90%) and bacterial media were purchased from HiMedia Laboratories Private Limited, Nasik, India. Methicillin Resistant Staphylococcus aureus (RHCC 3163) and Staphylococcus aureus (RHCC 2011) strains of bacteria were obtained from Rashid Hospital Microbial Culture Collection (RHCC), Rashid Hospital, Dubai, United Arab Emirates. Methicillin Resistant Staphylococcus aureus and Staphylococcus aureus were sub cultured from their respective stock culture and was sustained on Nutrient agar and Mannitol salt agar (MSA).
2.1 Antibacterial studies
Gram positive Methicillin Resistant Staphylococcus aureus bacteria (RHCC 3163) and Staphylococcus aureus strains of bacteria(RHCC 2011) were obtained from Rashid Hospital Microbial Culture Collection (RHCC), Rashid Hospital, Dubai, United Arab Emirates. Methicillin Resistant Staphylococcus aureus and Staphylococcus aureus were sub cultured from their respective stock culture and was sustained on Nutrient agar and Mannitol salt agar (MSA).
2.2 Preparation of Drug Solution & Formulation for Antibacterial studies
For antibacterial studies, levofloxacin plain drug solution and combinations with chitosan and chitosan with EDTA were prepared in final concentrations of 1024 μg/μl,512 μg/μl, 256 μg/μl, 128 μg/ μl, 64 μg/μl, 32 μg/μl, 16 μg/μl, 8 μg/μl, and 4 μg/μl after sufficient dilutions.Nutrient Agar media was also prepared, autoclaved and cooled at 50°C and appropriate amount was plated in sterile petri plates under sterile conditions. The plates were allowed to cool and were refrigerated and used the next day.
2.3 Determination of MIC by broth dilution method
MIC (minimum inhibitory concentration) and MBC (minimum bactericidal concentration) were determined by broth dilution method as reported earlier [30].Inoculum was acquired from an overnight nutrient agar culture of the experimental organism. Inoculum for the MIC test was prepared by taking at least three to five well-isolated colonies of the same morphology from an agar plate culture. The top of each colony was touched with a sterile loop and the growth was transferred into a tube containing 15 ml nutrient broth and incubated at 370C until it achieved the turbidity of the 0.5 McFarland standards correspond to bacterial population of approximately 2×108 cfu/ml. From this, 0.5ml of bacterial culture and 4.5 ml Mueller Hinton Broth was added to different concentrations of drug and incubated for 24 hours at 370Cto determine MIC and MBC.
2.4 Time kill analysis
Experiment for the rate of killing of the bacteria (SA and MRSA) by the LF+CH+EDTA were carried out using a modified time kill analysis technique of Eliopoulos and Eliopoulos and Eliopoulos and Moellering [31,32]. The nanoparticle was combined into 5 mL Mueller Hinton broth in sterile test tubes at 2×MIC and 4×MIC. The test tubes were incubated at 37°C. A 100 μL sample was removed from the culture medium at various time intervals from 0 – 24 hours for the determination of cfu/mL by measuring optical density and by the plate count technique [33] by plating out 25 μL of each of the dilutions on Nutrient agar.
After incubating at 37°C for 24 h, growing bacterial colonies were counted, cfu/mL calculated and compared with the count of the culture control without nanoparticle.
2.5 Animal Studies
Albino rats of either sex weighing between 200-250g from Lootah Technical centre, were used for the present investigation. Research and Animal Ethics Committee of Dubai Pharmacy College approved experimental protocol. The rats were housed at controlled temperature (25±2°C) and 12hrs dark-light cycle and provided basal diet in the form of pellets, water ad libitum.
The rats were randomly divided into 3 groups of 3 animals each. First group was kept as control, without any treatment. The second group was treated with 0.1% w/w LF formulated in 5% Hydroxypropyl methyl cellulose (HPMC) gel base. The third group was treated with 0.1% LF+CH+EDTA in 5% HPMC gel base.
MRSA skin infection animal model was used as reported earlier with slight modification [34]. The back of the rats were shaved and then mild burns were produced on their dorsal part under anesthesia (diethyl ether) with the help of heated rod. After cleaning the underlying skin with normal saline, the bacterial suspension containing approximately 2×108 cfu/ml of MRSA was applied on the burn skin with the help of sterile loop to produce MRSA skin infection and rats were kept 1 day without treated to observe visible growth of the bacteria. On the day 1, diameter of infected area was taken using vernier caliper and approximately, 0.5gm of LF gel and LF+CH+EDTA gel were applied to the respective groups. Control group was left untreated. The same procedure was repeated till Day 7.
2.6 Histological Studies of Infected Skin
The small portion of the skin were collected from the infected area of the animals on the last day of the experiment (Day 7) and preserved in 10% buffered formalin. Series of 3 - 4 μm thickness sections were prepared and stained with hematoxylin-eosin and photographed under 100x or 450x magnification. The rate of re-epithelialization, skin structure and inflammatory cells were evaluated by a blind histopathologist.
3. Results & Discussion
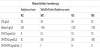
Minimum Inhibitory Concentration (MIC) and Minimum Bactericidal Concentration (MBC) were determined by means of standardized procedures. Levofloxacin in combination with chitosan and EDTA put forth an MIC of 16 μg/ml and MBC of 32 μg/ml on MRSA, whereas an MIC of 4 μg/ml and MBC of 8 μg/ml on SA (Table 1). LF+CH+EDTA exerted bactericidal effect against SA even at much lower concentration (8 μg/ml) compared to resistant strain MRSA (32 μg/ml) (Table 1).
In comparison, LF+CH exerted an MIC of 64 μg/ml and MBC of 128 μg/ml on MRSA, whereas an MIC of 32μg/ml and 64 μg/ml on SA and an MBC of 8 μg/ml. Levofloxacin alone on the other hand exerted an MIC of 128 μg/ml and MBC of 256 μg/ml on SA, whereas an MIC of 256 μg/ml and 512 μg/ml on MRSA.
The time kill analysis is used to determine the bactericidal or bacteriostatic activity of antibacterials. Bactericidal effect of LF+CH+EDTA was assessed by time kill studies which showed that at its 2× MIC (32 μg/ml) and at 4×MIC (128 μg/ml) concentration for MRSA, the LF+CH+EDTA initiated significant decrease in the amount of bacteria (Figure 1). For both the concentrations complete killing of MRSA was observed after 6 hours of incubation. The killing effect was noticeable with MRSA where >2 log reduction were observed in 4 h post treatment.
Diameters of infected skin patches are recorded in Figure 2 and repeated measures ANOVA followed by post hoc analysis was performed on the data using SPSS software. Difference on each day of treatment between control and LF treated, control and LF+CH+EDTA treated and LF and LF+CH+EDTA treated groups were individually compared using post hoc analysis.
Aliasgar F. Significant differences (p<0.05) between the diameters of the infected patch amongst the animal groupswere found by ANOVA. Post hoc analysis suggest there is significant difference between control and LF+CH+EDTA treated group and plain drug and LF+CH+EDTA treated groups, however, there was no significant difference between control group and plain drug treated group. When results on individual days of treatment were compared using student’s t test, there is no significant difference (p > 0.05) between control and plain drug treated group on all the days of treatment. While, significant difference (p < 0.05) on all the days of treatment starting from the first day was observed between control and LF+CH+EDTA treated group and plain drug and LF+CH+EDTA treated groups. Plain drug formulation shown little effect only from the 5th day of treatment, however, the reduction was not significant (p>0.05). LF+CH+EDTA treated group showed significant reduction in the diameter of infected area on animal skin from Day 1 of the treatment (p < 0.05) compared to both control and plain drug treated group and complete absence of the infected area was observed after 4th day of treatment.
The slides of skin sections were shown in Figure 3. The skin structure was found be normal in all the groups due to mild skin burn, epidermis layer was more or less intact. The presence of leukocytes in control group is indicating the infection in the dermis layer. However, in LF treated and LF+CH+EDTA treated groups, leukocytes were absent. Although, leukocytes were found absent in plain drug treated animals, visible observation of skin suggested the skin infection. However, in case of LF+CH+EDTA treated group both the visible observation and histopathological study (figure 4) suggest no infection proves complete eradication of bacterial infection.
4. Discussion
Antibiotic resistance is one of the greatest threats to modern health and most of the bacteria are developing increased resistance to antibiotics. The present study demonstrates the effectiveness of LF in combination with CH and EDTA (LF+CH+EDTA) against both methicillin sensitive and methicillin resistant S. aureus both in vitro and in vivo. Levofloxacin alone showed MIC of 128μg and 256μg against SA and MRSA respectively. The mechanism of action of levofloxacin is inhibition of bacterial topoisomerase IV and DNA gyrase, enzymes required for DNA replication, transcription, repair and recombination. MRSA bacteria are almost found to be resistant to multiple antibiotics. When combined with chitosan in equal concentration, one-fold log2 reduction in MIC against MRSA and two-fold log2 reduction in MIC against MIC was observed. No reduction in MBC concentration was observed in case of MRSA. The exact mechanism for antimicrobial properties of chitosan is still not very clear, however, the interaction of positively charged molecules of chitosan with anionic components of microorganisms, lipopolysaccharides (Gram-negative bacteria) and teichoic acid (Gram-positive bacteria) are considered to be the main reasons [35-40]. Therefore, acidic conditions are required for antimicrobial activity of chitosan since amino groups are ionized only at acidic pH [41,42]. Also, chitosan's in vitro antimicrobial activity depends on many factors, such as degree of deacetylation, molecular weight of chitosan, its concentration in a solution, or pH and the ionic strength [43]. However, chitosan's activity is mostly growthinhibitory, where resistant subpopulations might emerge; as a result of physiological adaptation of the cells to chitosan stress [44].
Reports suggest that chitosan antimicrobial activity is markedly increase by addition of EDTA [45-48]. When drug and chitosan solution was combined with EDTA in equal weight ratio, the MIC and MBC concentrations were three-fold log2 and two-fold log2 reduction in MIC against MRSA and MSSA was observed. A study conducted in 2011, evaluated antimicrobial activities chitosan-EDTA combination against Gram-negative and Gram-positive bacteria as well as Candida albicans. EDTA failed to have inhibitory activity against Enterococcus faecalis, a gram positive bacteria, as well as MBC against any of the studied microorganisms. However, chitosan- EDTA combination demonstrated synergistic antimicrobial activity against Staphylococcus aureus and an additive effect against other microorganisms [49].
The results of antimicrobial studies were further confirmed by animal studies. LF+CH+EDTA combination showed significant reduction in the diameter of infected area on animal skin from Day 1 of the treatment (p < 0.05) compared to both control and plain drug treated group and complete absence of the infected area was observed after 4th day of treatment.
Thus, it can be concluded that antibiotic with chitosan and EDTA combination is a potential drug delivery system to overcome antibiotic resistance in MRSA and MRSA skin infections. However, further studies with other antibiotic resistant bacterial strains need to be conducted to generalize the applicability of the developed formulation in overcoming antibiotic resistance.
Competing Interests
The authors declare that they have no competing interests.