1. Background
Children with cerebral palsy (CP) commonly require long-term treatment to increase their functional abilities and maintain their independence. One community-based program that has been shown to be beneficial and enjoyable to children with CP is therapeutic horseback riding (THR). THR utilizes the rhythmic, variable, and repetitive movement of a horse to provide sensory input to the rider that mimics normal movement patterns of the human pelvis during walking [1]. The horse’s gait challenges vestibular, proprioceptive, and visual senses that promote increased trunk strength/control, balance, posture, and motor planning [1]. The horse’s 3-dimensional movement creates perturbations to the rider’s center of gravity in the sagittal, frontal, and transverse planes of movement [2]. Maintaining balance and proper posture while on a horse requires minute, subtle positional adjustments and challenges the rider to utilize unfamiliar but natural movement patterns. It is a task-oriented intervention that encourages the rider to discover his own solutions for improving postural control [2,3] Therapists can position the child atop the horse in various positions such as prone, side sitting, or forward sitting [2,4]. The child may also perform a variety of tasks such as reaching, twisting and turning.
Most THR programs can last anywhere between 8-12 weeks with waiting lists for the service commonly occurring. The majority of the research on THR has focused either on the functional outcomes of a long-term riding interventions that last 8-10 weeks, or the physiological influence of a short-term riding interventions lasting only minutes.
In 2003, Benda and McGibbon et. al. evaluated the effects of 8 minutes of hippotherapy compared to 8 minutes of barrel riding in children with cerebral palsy [5]. 15 children were randomized into either a hippotherapy or a barrel riding session for only 8 minutes. Results showed significant improvement in symmetry of muscle activity in muscle groups displaying the highest asymmetry. No significant change was noted after barrel riding [5].
In 2009, McGibbon and Benda et. alcreated a follow-up study that investigated the effects of short-term vs. long-term hippotherapy intervention on the symmetry of adductor muscle activity during walking in children with CP. Phase I examined the immediate effects of 10 minutes of hippotherapy compared with 10 minutes of barrel sitting and demonstrated significant improvement. Phase II examined the effects of hippotherapy offered once a week for 12 weeks and demonstrated significant gains in several functional domains that were sustained for 12 weeks posttreatment [6].
Drnach et. al. investigated the effect of a short-term therapeutic riding program on the gross motor function in a child with cerebral palsy [7] One subject participated in a 5-week therapeutic horseback riding program consisting of 1 hour of riding per week. Results showed that improved scores on the Gross Motor Function Measure in two of the five dimensions measured and scored. To date, this is one of the few studies that evaluated THR intervention for a time period less than 8 weeks [7].
The purpose of this study is to determine if a single one-hour session of therapeutic horseback riding significantly improves the GMFM score of a child with cerebral palsy.
2. Case Description
A single subject repeated measures case study design was used forthis study. It implemented two pretests and one posttest, using the GMFM as an outcome measure, comparing scores before and after a single session of THR.
A diagnosis of Ante-partum eclampsia in an unbooked primigravida was made. Other differential diagnoses noted were cerebral malaria and meningitis. Blood sample was taken for complete blood count and differentials; rapid diagnostic test for malaria parasite (Paracheck), and blood slide for malaria microscopy was also taken butno parasites were seen, random blood sugar and urinalysis were also conducted. The results of the investigations are displayed in Table 1.
Subject: The medical director of an outpatient center that provides THR identified the subject for this study. The inclusion criteria included: (1) interest in the facility’s THR program, (2) has a diagnosis of cerebral palsy, (3) is affected by no other medical complications such as uncontrolled seizures, (4) has the functional ability to sit and stand alone or with support, (5) has the consent from parents, (6) is able to follow simple one-step directions, and (7) is between the ages of 3 and 16 years of age. Exclusion criteria included: (1) severe uncontrollable behavioral problems, or (2) had orthopedic or neurologic surgery in the previous 6 months.
The subject chosen for this study was a 9-year-old white boy with a diagnosis of CP, spastic diplegic presentation, GMFCS Level I, with no history of THR. He attends public school and participates in a regular education program. He is an only child from an upper-middle class family and lives with both parents. He wears bilateral ankle foot orthotics (AFOs) with articulating ankle joints, posterior check strap and soft inserts for 8 hours a day. He has a history of soft tissue lengthening in the lower limbs including Achilles tendon lengthening and adductor muscle lengthening. He was on no medication during the time of the study. His parents accompanied him to the THR session and all data collection sessions. Riding took place in an outdoor arena on a horse that had prior experience in the THR program. The child was required to wear a helmet and was supported by 2 side walkers and one leader. The leader was an experienced handler and led the horse at a walking pace while the child followed the commands of the instructor who placed herself at the center of the arena. Riding was completed with the use of a western saddle and the child was permitted to use the reins and provide verbal cues such as “whoa” and “walk on” to his horse. A safety belt with two handles was placed around the child’s waist for the side walkers to grasp for safety while riding.
IRB approval for this study was obtained from the participating institutions. Consent of the child’s parents and assent of the participating child were also obtained.
Instrumentation: The GMFM was used to assess the child’s functional ability throughout the duration of the study [8]. It was chosen based on the following: (1) clinical relevance and sensitivity of the test specific to changes in motor function, (2) the amount of time required to complete the test, (3) the reliability of the GMFM, providing consistent scores when used repeatedly with the same subjects, and (4) the validity of the measure [8]. The researcher recorded the child’sscore for each functional dimension for the pre-test and post-test data. Dimensions included: (A) Lying and Rolling, (B) Sitting, (C) Crawling and Kneeling, (D) Standing, (E) Walking, Running, and Jumping.
An IPad © by Apple was used to record the child performing the functional tasks of the GMFM during each scheduled session of data collection. Three videos were gathered, each representing pre-test 1, pre-test 2, and post-test 1 respectively. The videos were used to verify the child’s execution of the test items to assure that the scores obtained during the data session were accurate.
Procedures: The GMFM was used to assess the child in 2 separate sessions; two days before and one day prior to the initiation of the intervention. GMFM testing was completed in the same room and with the same equipment each time. Measurements were performed and scored by a physical therapist trained and qualified in the administration of the GMFM. All 88 movements were performed during the first session of data collection to establish a baseline. The second session was conducted to capture any change in score due to repeated performance. The second and third sessions tested only walking, running, and jumping movements since the child scored a 100% in the supine, sitting, crawling, and standing GMFM dimensions during the first testing session.
After two sets of GMFM scores were obtained, the child participated in one session of therapeutic horseback riding. The session lasted one hour and began with the child and his team of side walkers completing a few laps around the arena, changing direction a few times. The child was joined by about 4-5 other riders who all would standby and listen for instructions from the riding instructor. Once instructions were delivered, the children would perform the task to the best of their ability.
The riders and their horses were led over rails and through orange cones in a serpentine pattern to challenge the rider’s sense of balance and proprioceptive abilities. Riders were also asked to twist, turn, and reach outside their center of balance in order to successfully throw a ball into a bucket and also pass a toy down an assembly line with the other participants in the riding session. Within two hours after the THR session was completed, the child was tested with the GMFM one more time to obtain data post-therapeutic riding session.
3. Outcomes
The child was allowed a maximum of three trials on each item. Percentage scores were calculated within each dimension and averaged to obtain a total score that ranges from 0 to 100.To determine the goal total score, only the dimensions identified as goal areas by the clinician are included – these are the areas where greatest change is expected to take place [11]. This helps to increase the responsiveness of the measure.
The child’s home was used as the testing site. This is consistent with the following test related criteria: the GMFM should be administered in an environment that is comfortable for the child. It is important to keep the environment for the testing as consistent as possible for each administration of the measure [9].
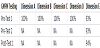
Three sets of GMFM scores were analyzed and compared to determine differences in the child’s gross motor function as a result of a single therapeutic riding session. (Table 1) Each dimension of the GMFM was assessed and differences between the three were recorded. The video of the child’s performance was also reviewed to verify his performance with each testing session.
In the first pretest, the subject scored a 100% in the Dimensions (A) Lying and Rolling, (B) Sitting, (C) Crawling and Kneeling, and (D) Standing, and 93% on Dimension (E)Walking, Running, and Jumping. Dimension E was identified as the only goal area and focus of the data analysis because the subject scored 100% on Dimensions A, B, C, and D. The initial score in Dimension E was attributed to the subject’s inability to successfully complete the criteria to run effectively, to hop 10 times within a 2-foot circle/area, and to jump up 12 inches high. On the second pretest, performed two days later, he scored a 93% on Dimension E.
On the posttest, held after his first THR session, the subject scored a 94% on Dimension E. These improvements were based on his ability to initiate hopping in place while remaining within a 2-foot circle/area although his foot did not consistently leave the ground.
GMFM items which the subject could partially complete included Item 80: jumps 12 inches high both feet simultaneously, Item 82: Standing on one foot (both right and left respectively) and hopping 10 times within a 2-foot circle/area.
4. Discussion
This study provided objective data on the effects of one session of THR on the gross motor function of a child with cerebral palsy. The child demonstrated only a slight change in his GMFM score in Dimension (E) Walking, Running, and Jumping. These motor activities require significant strength, balance, coordination, specific weight-shifting ability, and postural support to be completed efficiently. Although this study showed an improvement in Dimension E Walking, Running, and Jumping, the subject’s increase in gross motor function was not considered significant.
Determining the appropriate amount of intervention to produce a significant change can result in the more efficient utilization of the resource. Literature has shown that one session per week for 5 to 8 weeks can produce a change in a child’s gross motor function. This study suggests that a child needs greater than one session in order to produce that change.
One benefit of determining the optimal level of THR intervention may be the reduction of waiting lists as a result of participants circulating faster through the program while receiving the same physical benefits. If an efficient number of THR sessions can be discovered that produces a measurable change in children with CP, then THR can become more efficient and cost-effective.
Competing Interests
The authors declares that there is no competing interests regarding the publication of this article.
Acknowledgments
The authors would like to thank the Easter Seals Rehabilitation Center in Wheeling, WV and Ellen Kitts, MD for their involvement and assistance with this project.