1. Introduction
There are increasingly more adults being diagnosed with attentiondeficit hyperactivity disorder. The most common initial treatment is the institution of a stimulant medication. In those patients who do not abuse the medication and who have no underlying predisposition to develop psychosis such as those with bipolar disorder or schizophrenia, stimulant-induced psychosis on therapeutic dosing has not been reported significantly in the literature. The following case is one of a patient who, despite complying with dosing instructions, developed florid psychosis requiring hospitalization and treatment as a result of taking stimulant medication for ADHD. It is important for those who practice adult medicine and psychiatry to understand that this is a potential reaction to this medication. The following study also discusses alternate medications and treatment modalities for treating the disorder that do not include the use of stimulants.
2. Case Presentation
Our patient is a 26 year old male with no prior psychiatric history who self-presented to our outpatient mental health clinic with a chief complaint of difficulty focusing in school. The patient was taking physical therapy classes. He stated that he would do well in math because it required understanding, but would not be able to focus to recall information for English and history, the former of which he had dropped. He had recalled being fidgety in school, but denied being a “class clown” or having had discipline problems. He did endorse some problems in school, but had no history of learning disabilities. He was told that he was “hyper” when he was younger, and he had recalled having taken a friend’s Adderall which had helped him to focus better. Yet he had never been evaluated for ADHD. His grades worsened after his freshman year, and patient reported that he has barely been able to graduate from high school. The patient was ultimately diagnosed with ADHD in our clinic based on self and parental reports.
Initially Ritalin was prescribed twice daily, but he felt anxious and “odd” on the medication after 4 weeks duration. So he was prescribed Adderall at 20 mg twice per day, and soon after, the dosing was increased to 20 mg three times per day, a dose he had been on for about 2 weeks prior to his subsequent presentation to the emergency room.
On presentation, he was disorganized, paranoid, and referred to recent encounters with aliens whom he reported were visiting him on a regular basis to impart information. His wife had reported that he had had milder symptoms on several occasions, weeks prior, with some disorganized thought and agitation that had improved with sleep. He was admitted to inpatient psychiatry and was started on olanzapine at 20 mg daily. Over the course of his four day hospitalization, his thought process became more organized and reality based, and the patient was discharged home on a short course of nightly olanzapine. His symptoms resolved completely. The patient was ultimately placed on atomoxetine in conjunction with behavioral therapy to manage his symptoms and has had no relapse in symptoms.
3. Discussion
There is clear evidence that ADHD symptoms continue into adolescence and adulthood with an adult prevalence of anywhere from 3% to 7% [1, 2]. Research has demonstrated a significant relationship between ADHD symptoms and one’s ability to function in daily life. Problems with inattention such as losing or forgetting things have a negative effect on critical areas in one’s personal life including an impact on personal relationships, on academic and life skills, all while increasing participation in risky activities and leading to erratic and unsafe driving [3]. Adults not only have lower levels of education when they suffer with attention problems, but they have a difficult time obtaining and maintaining employment. Treatment can address many of these issues [4].
There are some challenges in diagnosing ADHD in adults. Just as in children, adults with ADHD are noted to be forgetful and have organizational problems. However, because adults have greater planning demands placed on them, their symptoms can become increasingly prominent, but yet manifest differently. Frustration, poor motivation, procrastination, overreaction to frustration, and problems with time management are common complaints, but are not criteria addressed in the DSM-V. It may be that the criteria and diagnostic thresholds for adults are inappropriately worded and too restrictive, respectively, to consistently identify adults with ADHD. Adults will seek treatment because of problems with productivity, frustration, and impairments in quality of life. Unlike children who struggle with demands during the day while at school, adults often have challenges at both home and at work and are affected in more domains in their life. A comprehensive clinical interview, behavioral rating scales, family history, or neuropsychological testing can all assist in making an accurate diagnosis. Our patient appeared to have met criteria for this condition and was challenged enough in his daily life because of his symptoms that pharmacologic treatment was appropriate [5].
Stimulants are not only FDA approved, but are the treatment of choice in managing ADHD with medication. They make patients more alert and improve concentration, all while decreasing aggression and impulsivity. These drugs, which are thought to act by causing a release of both norepinephrine and dopamine, are considered to be both safe and effective. Multiple double blind controlled placebo trials have demonstrated that adult patients will have a response to methylphenidate and mixed amphetamine salts, with response rates ranging from 25% to almost 80% [6-8].The availability of longer lasting preparations of methylphenidate and mixed amphetamine salts in extended release versions, permits a substantial decrease in dosing frequency, which was often thrice daily, and can be reduced to daily given that newer formulations now last six to twelve hours. Initial dosing can be increased weekly for desired symptom control with most agents at maximum dosing by four weeks. Side effects include nervousness, appetite suppression, insomnia, an increase in heart rate and blood pressure, irritability and dysphoria, and rebound. About 30% will not respond or are not able to tolerate stimulants [9]. However, before a treatment failure defined as inadequate symptom response to stimulants is considered, patients who are started on methylphenidate should be tried on mixed amphetamine salts as a significant response can still be achieved on the latter. In our patient, overt psychosis limited the use of an alternate stimulant.
Amphetamine induced psychosis is characterized by prominent visual hallucinations, parasitotic delusions, anorexia, flattened affect, and insomnia. The mechanism of amphetamine induced psychosis is thought to be due to an excess of dopamine, such as that noted in schizophrenia. Amphetamines release dopamine directly from newly synthesized pools of the neurotransmitter. Controlled studies in hospitals have demonstrated the induction of psychotic symptoms when patients were given small hourly doses of amphetamines. The patients had progressive flattening of affect and anhedonia followed by psychotic states. Psychotic symptoms generally lasted between 1 to 6 days, but in one patient persisted for nearly a month. Animal studies show that when animals become psychotic in response to administration of amphetamines, they will readily have symptom relapse after a single re-administration dose [10,11]. Whether our patient was experiencing his first psychotic break or had a reaction to his medication remains to be seen, but the latter is more likely given the timing of his symptoms and the rapid clearing and cessation of symptoms when the medication was stopped.
There are alternative pharmacologic therapies for treating ADHD. Double blind controlled trials demonstrating that between half and two-thirds of patients will show a clinically significant response to bupropion and desipramine are well known. Bupropion likely has both indirect dopamine agonist and noradrenergic properties [12]. Tricyclics decrease both norepinephrine and dopamine re-uptake. Venlafaxine also has proven effective in open label trials and has both serotonergic and noradrenergic effects [13,14]. Desipramine has the most research behind it in terms of demonstrating efficacy, followed by atomoxetine.
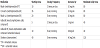
Atomoxetine, a specific norepinephrine re-uptake inhibitor, is the first drug that has been approved by the FDA specifically for the treatment of ADHD in adults (Table 1). It has several distinct advantages. It is a non-stimulant and highly specific norepinephrine reuptake inhibitor. There is less rebound with this medication, and once per day dosing provides complete daily coverage into the evening. The drug also has mild anti-depressant effects. In those patients in whom there is a strong history of substance use or for those who are anxious about taking as a stimulant, this is the drug of choice. Side effects include dry mouth, nausea, decreased appetite, constipation, decreased libido, dizziness, decreased sex drive, erectile dysfunction, and dysuria [15].
While clonidine and guanfacine have been evaluated in the treatment of children with ADHD, their effectiveness in adults has not been studied adequately to make a determination. These medications are thought to inhibit norepinephrine release and increase dopamine turnover, all while reducing serotonin levels. Taylor and Russo demonstrated that guanfacine did reduce ADHD symptoms in adults, but more research is needed [17].
The importance of environmental restructuring cannot be underestimated even in the context of medication management. Individualized instruction versus group learning can help patients to compensate for the problems that they have with executive function. Programs designed to teach time management, sleep strategies, and organizational skills can be very useful. Cell phones and other computerized devices may help patients with attention, planning, and time management. Patients can be taught how to self-monitor and experiment in order to create better work flows and coping strategies during the day [16,18,19].
4. Conclusion
Patients taking stimulants for the treatment of ADHD may be at risk of developing psychosis. Until these risk factors are clarified, it is important for all practionersto take a careful psychiatric personal and family history for schizophrenia. It is also essential that patients be monitored closely on initiation of treatment and during induction for behavioral changes, all while emphasizing the importance of taking drugs as prescribed in order to avoid the development of psychosis.
Competing Interests
The authors have declared that no competing interests exist.
Author Contributions
Mary Gable wrote up the case, performed a literature review, and wrote the article.
Dwayne Depry assisted with revisions and well versed in the hospital course of this patient. All authors read and approved this final manuscript.