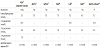
Gestational diabetes mellitus (GDM) is defined as carbohydrate intolerance of varying degrees of severity with onset or first recognition during pregnancy [1]. This clinical entity was first identified in 1957 by Carrington and his colleagues, but the diagnosis of GDM was formalized by John O’Sullivan through the 3-hour 100g glucose tolerance test (OGTT) [2-4]. The authors assessed the distribution of plasma glucose levels in pregnant women, and determined the diagnostic threshold for GDM. The initial rationale for diagnosing GDM was to assess the risk of women in developing post-partum diabetes, but there was also some data linking GDM to adverse pregnancy outcomes [4]. Since then, there had been a number of diagnostic criteria for GDM (Table 1) [5-9]. This had resulted in a great deal of confusion among clinicians, and the lack of standardization of diagnosis of GDM also made it difficult to compare women with GDM between different countries. A number of studies had confirmed that treating women with GDM resulted in better obstetric outcomes, and therefore making the diagnosis of GDM is highly relevant [10,11].
Abbreviations:
ADA: American Diabetes Association
ADIPS: Australian Diabetes in Pregnancy Society
NZSSD: New Zealand Society for the Study of Diabetes
WHO: World Health Organization
CDA: Canadian Diabetes Association
EASD: European Association for the Study of Diabetes
1. Fasting glucose or glucose challenge test as screening tests
In some regions in the world, GDM screening is only performed in pregnant women with risk factors [12]. These risk factors included body mass index above 30kg/m2, previous macrosomia, previous GDM, women with family history of diabetes and belonging to certain ethnic groups [12]. However, women with no risk factors can develop GDM, and the outcomes are no different in women identified by risk factors [13]. Screening based on risk factors may fail to detect up to 40% of women with GDM, and hence there are merits for universal screening if resources are available [13,14].
Because performing 75g or 100g OGTT on all pregnant women is time consuming and expensive, a 2-step approach is often adopted in many countries for diagnosing GDM. A screening test, such as the 1-hour 50g glucose challenge test (GCT), was advocated by Coustan and his colleagues [15]. GCT as a screening test does not involve fasting and can be done at any time of the day. In Coustan’s study of 6000 women screened with GCT, an abnormal threshold of 7.8mmol/L (140mg/dL) was set, above which the women would proceed to OGTT. A threshold of 7.8mmol/L (140mg/dL) would give a sensitivity of 80%, and about 15% of women would need to undergo OGTT. Lowering the threshold to 7.2mmol/L (130mg/dL) would increase the sensitivity of the screening test but more women would have to undergo OGTT (about 25%)[16]. Studies had shown that when the glucose value following GCT exceeded 11mmol/L (198mg/dL), the likelihood of GDM is very high and the woman may not need to proceed to the full OGTT [17].
Fasting plasma glucose (FPG) was also used as a screening test for GDM. In a study of 1465 women who underwent FPG as well as 75g OGTT, a FPG threshold of 4.7mmol/L (85mg/dL) would exclude GDM in almost 50% of women, but would miss about 14% of women with GDM [18]. In another study, if a cut-off FPG value of 4.4mmol/l (79mg/dL) was chosen to rule out GDM, a sensitivity of 94.7% was attained [19]. When comparing GCT with FPG, a study of 188 women found that GCT yielded a better specificity than the FPG and the FPG for a comparable level of sensitivity [20]. In studies that examined cut-off values for GCT or FPG, the sensitivity and specificity of these screening tests were highly dependent on the ethnicity of the population, local prevalence of GDM as well as the GDM diagnostic criteria selected for that region.
2. HAPO Study and IADPSG recommendations
The Hyperglycaemia and Adverse Pregnancy Outcome (HAPO) study was a large international study involving over 25,000 women that assessed the effects of maternal glycaemia at 24-32 weeks’ gestation on pregnancy outcomes [21]. There was a linear association between fasting, 1-hour and 2-hour glucose levels on the 75g OGTT and various clinical and biochemical peri-natal outcomes (including birth-weight >90th percentile, cord C-peptide >90th percentile and neonatal body fat >90th percentile). The study was conducted in centres across North America, United Kingdom, Israel and Australia, but notable omissions included India, sub-Saharan countries and China (except Hong Kong).
To discuss the results from HAPO and other studies, the International Association of Diabetes in Pregnancy Study Group (IADPSG) held an International workshop-conference in 2008 in Pasadena, California. Using an odds ratio (OR) of 1.75 for those pre-specified pregnancy outcomes, the working party determined the thresholds glucose levels for diagnosing GDM. Based on these calculations, the IADPSG consensus panel proposed the implementation of a new diagnostic criteria with threshold fasting glucose at 5.1mmol/L (92mg/dL), 1 hour glucose at 10.0mmol/L (180mg/dL) and 2 hours at 8.5mmol/L (153mg/dL) following 75g OGTT [22]. GDM is diagnosed when one or more of these threshold glucose levels are exceeded. Using these cut-off values, 17.8% of the women in the HAPO cohort would have been diagnosed with GDM. This was compared to a GDM incidence of 25% when OR of 1.5 was used, and 8.8% if OR of 2.0 was chosen.
In their recommendations, the panel suggested performing 75g OGTT in all pregnant women at 24-28 weeks’ gestation, rather than risk-based screening. For women who are deemed to be at high risk for GDM, they should be excluded for overt diabetes and this can be assessed with fasting glucose level, random glucose or glycosylated haemoglobin at the initial antenatal visit. In their recommendations, there was no mentioned of whether GCT may still have a role.
3. Diagnosis of GDM world-wide following IADPSG recommendations
The IADPSG recommendations were adopted in some countries but rejected by many others. The World Health Organization (WHO) in 2013 had published a revised definition of diabetes in pregnancy, accepting the IADPSG recommendations for the diagnosis of GDM [23]. In United States, the American Diabetes Association (ADA) supported the IADPSG recommendations in 2011. However, the National Institutes of Health (NIH) held a consensus development conference to discuss the diagnosis of GDM in March 2013, and a draft statement stated that the NIH panel did not find sufficient evidence to support a 1-step approach proposed by IADPSG [24]. Furthermore, the American College of Obstetricians and Gynaecologists is yet to endorse the IADPSG recommendations. The Canadian Diabetes Association expert committee in 2013 adopted the preferred approach of sequential screening with a 50g GCT followed by a 75g OGTT using the glucose thresholds that result in an OR of 2.00 for pregnancy outcomes [25]. Interestingly, the expert committee stated that an alternative approach using a 1-step 75g OGTT based on IADPSG criteria was also acceptable [25].
In Asia, the Japanese Diabetes Society and Chinese Diabetes Society had both adopted the IADPSG recommendations for the diagnosis of GDM [26,27]. The Chinese Ministry of Health stated that this 1-step approach was appropriate for well-resourced institutions [28]. However, in rural areas or in poorly resourced institutions, FPG could be performed as a screening test. If the FPG was below 4.4mmol/L, GDM was considered unlikely, while women with FPG between 4.4 and 5.1mmol/L should still proceed to 75gOGTT. On the other hand, India had not taken up the IADPSG recommendations. The Diabetes in Pregnancy Study Group India (DIPSI) has persisted with a 1-step approach at 24-28 weeks’ of gestation where GDM is diagnosed when the 2-hour glucose level exceeded 7.8mmol/L (140mg/dL) following 75g of glucose load, with no diagnostic threshold for FPG [29,30].
In Oceania, the Australian Diabetes in Pregnancy Society (ADIPS) and the Royal Australian New Zealand College of Obstetricians and Gynaecology (RANZCOG) had both endorsed the IADPSG recommendations, and advocated for universal 1-step testing of pregnant women at 24-28 weeks’ gestation [31,32]. ADIPS also specifically stated that GCT should not be used, as it was considered to “lack sensitivity and specificity and will no longer be part of the diagnostic algorithm for GDM”. The RANZCOG council meeting further asserted that up to 25% of GDM is missed by the 2-step process when using GCT as the screening test first.
The Diabetic Pregnancy Study Group (DPSG) of the European Association for the Study of Diabetes (EASD) had not recommended any change to the diagnostic criteria for GDM. Within various European countries, however, their screening strategies differ widely. Austria and Italy has adopted the IADPSG diagnostic criteria, whilemany other countries still use the old World Health Organization diagnostic criteria (FPG ≥ 7.0mmol/L or 2-hour glucose level ≥ 7.8mmol/L on 75g OGTT).
4. Where to from here?
It has been 4 years since the IADPSG recommendations were published, yet the uptake of their diagnostic criteria internationally has been mixed. There are a number of reasons for not endorsing these recommendations. Firstly, the choice of using OR of 1.75 for adverse pregnancy outcomes in determining the glucose thresholds for GDM diagnosis is still being debated. Secondly, implementation of a universal screening, rather than risk factor based testing, will impose substantial burden on the health system in some countries. Prior to IADPSG recommendations, there were already well-established local protocols for detecting GDM and there is a great deal of resistance or inertia to change. To perform 75g OGTT on all pregnant women, it is anticipated that pathology services will be overwhelmed especially in the morning. From database reviews such as in Australia, an extra 30% of pregnant women will be diagnosed with GDM with the IADPSG guidelines, and this will significantly increase the workload for diabetes services [33]. There must be sufficient resources to not only diagnose GDM, but also to treat these women as well. Most of the diabetes services that are managing GDM are already functioning at or close to full capacity, and a significant increase in the number of women diagnosed with GDM will put great stress on existing staff and institution.
From the patient point of view, a screening test such as GCT is convenient as this can be done at any time of the day and takes up less time for the woman. In rural areas or in countries where women have to travel long distances to attend antenatal services, the 75g OGTT may be impractical. For a country to change the diagnostic criteria for GDM, this may require extra funding from the government, or involve major changes in the structure of current clinical practice. There is certainly a need for health economic modelling in each country to evaluate the cost-benefits for adopting the IADPSG recommendations. Interventional studies are also needed to establish whether treating women with GDM based on the IADPSG criteria will result in improved pregnancy outcomes.
Despite the many reservations held by some local diabetes leaders over the world, the IADPSG recommendations are still the most evidence-based among the various diagnostic criteria currently being utilized. The IADPSG recommendations reflect consensus view and the Pasadena meeting in 2008 was attended by 225 conferees from 40 countries. By unifying the diagnosis of GDM internationally, this would mean that pregnant women with equivalent glucose levels can be grouped in a similar manner, thus making collaborative research more feasible across different countries. This would also allow valid comparison of the incidences of GDM between different regions in the world.
Ultimately, each country needs to decide the most appropriate method to diagnose GDM for its people, taking into account factors such as resources, health infrastructure and local prevalence of GDM. Nevertheless, some form of glucose assessment is better than no screening at all, whether this is through 1-step or 2-step approach, and whether this is by using tools such as GCT, FPG or OGTT. The 75g OGTT is probably the most widely used tool at the moment, and if this test is chosen as the diagnostic test, currently the IADPSG recommendations offer the most sensible threshold values, and this may become the “gold standard” for diagnosing GDM.