1. Introduction
As interest in research on job-related stress in psychiatric nurses (PNs) has been increasing in recent years [1-3], we previously developed the Psychiatric Nurse Job Stressor Scale (PNJSS) that can assess job stressors that are unique to PNs [4]. The scale is comprised of 22 items in four categories of factors - psychiatric nursing ability, attitude of patients, attitude toward nursing and communication - extracted from among a total of 63 items in factor analysis (maximum likelihood measure, promax rotation and scree test). However, as we removed many items in the repeated factor analysis (FA), we identified, as a limitation of PNJSS development, that the PNJSS is not a final scale that can assess all the job stressors of PNs [4]. In FA, differences in factor extraction method, predicted number of factors and method for factor rotation can affect the results [5]. In particular, we used the scree test [6] in our previous study [4] to predict a number of factors for FA, which may have resulted in too many or too few factors [7,8]. The 41 items that were not selected in the previous study included four factors. In addition to the three factors from Ohnishi [9] that could comprise a general concept for job stressors that may be unique to PNs, we predicted new factors;(1) estimate of situation for psychiatric nursing, (2) physical environment of the psychiatric ward and (3) medical accidents in the psychiatric ward. The following is the basis of predicted three new factors.
A look at the current situation in psychiatric nursing care shows Japan to have not only the highest number of psychiatric care beds per 100 population, at 27.8 beds [10,11], but also the longest mean duration of hospital stay for psychiatric inpatients in the world [12]. Even with stable symptoms, there is no place for them in the community, resulting in over 70,000 patients in social hospitalization forced into long-term hospital stays [13]. When actually attempting hospital discharge support, PNs may find community care options for patients inadequate, making it difficult to predict the future lives of patients in psychiatric nursing care [14].
The physical environment in psychiatric wards in which PNs must provide nursing care is unique in that each area in the ward is locked for the patient’s and other patients’ safety [15-17]. While PNs feel that this type of environment has the advantage of enabling them to practice safe and efficient care, they also feel that it has the disadvantage of being a non-therapeutic environment that feels like a detention facility [16]. They may therefore be predicted to suffer stress due to the structure of the psychiatric ward.
Looking at medical accidents that are distinctive of psychiatric wards shows that delusions in psychiatric patients have a high risk of violence [18], and PNs are frequently aware of the possibility that patients may become violent [19,20]. PNs are therefore likely to have a higher burden from risk management in the psychiatric ward. PNs may carry a daily feeling of stress related to medical accidents that are distinctive of psychiatric wards.
It is therefore predictable that PNs have unique job stressors. However, original PNJSS cannot measure these job stressors. Developing a PNJSS (Supplemental version) may enable a more detailed assessment of job-related stress in PNs and enable the provision of even more useful information for self-care by PNs and supervised care by their supervisors.
We therefore set out to develop a PNJSS (Supplemental version) with a focus on estimate of situation for psychiatric nursing, physical environment of the psychiatric ward and medical accidents in the psychiatric ward and to test the reliability and validity of the scale.
2. Materials and Methods
2.1 Preparation of the questionnaire
To understand the basic characteristics of the participants, the questionnaire included spaces to write down their age, gender, job position, qualifications and experience of working in other departments. Then, 63 question items from our previous study related developing of the PNJSS [4], we selected total 11 question items of 4 items related ‘Estimate of situation for psychiatric nursing’, 3 items related ‘Physical environment of the psychiatric ward’ and 4 items related ‘Medical accident and unpredictable behaviors of psychiatric patients’, which we confirmed with a nurse and university faculties who had experience of working in a psychiatry department. There were no items that overlap with questions of PNJSS in this study. We paid attention to the following points in each question: (i) the subject and the predicate were unified as "I think- / feel-"; (ii) the verb tense was unified to the present tense; (iii) multiple sentences were not included in one question item. A Visual Analogue Scale (VAS) was used to record answers. A sentence instructed the respondents thus: “These questions refer to your present psychiatry department work. Please make a circle O on the place on the line that best matches your response.” The VAS was 100mm long, and points were set at every 1mm. For each question, the score was highest toward “Yes, I think/ feel so” and indicated a high job stressor. Appendix 1 shows the final version of the PNJSS (Supplemental version).
To examination of the validity in the PNJSS (Supplemental version), we used the Psychiatric Nurse Job Stressor Scale (PNJSS) developed by Yada et al [4],and the Job stressor (JSS) and Stress Reaction (SRS) scales from the Brief Job Stress Questionnaire (BJSQ) developed by Shimomitsu et al [21].The PNJSS was composed of Psychiatric Nursing Ability (9 items), Attitude of Patients (6 items), Attitude Toward Nursing (5 items) and Communication (2 items). The JSS was composed of quantitative overload (3 items), mental demand (3 items), physical workload (1 item), job control (3 items), and utilization of techniques (1 item), interpersonal relations (3 items), work environment (1 item), fit to the job (1 item) and reward of work (1 item). The SRS was able to measure the psychological and physical stress reaction scale. The psychological stress reaction scale was composed of lack of vigor (3 items), irritability (3 items), fatigue (3 items), anxiety (3 items), and depression mood (6 items). The physical stress reaction scale was composed of somatic symptoms (11 items). The BJSQ had sufficient reliability and validity in the development process [21].
2.2 Procedure
Anonymous self-administered questionnaires that had been sent by mail from November 17, 2009 to March 10, 2010 were investigated. To evaluate the test-retest reliability, the questionnaires of the same respondents were investigated twice. The first investigation period was from November 17, 2009 to December 21, 2009, and the second investigation period was from February 9, 2010 to March 10, 2010. The participants were informed of the aim of the investigation and their written informed consent was obtained. Part of the data from a previous study [4] also was used in the present study to develop the PNJSS (Supplemental version), although the aims and analysis of the studies were different. The study protocol was approved by the Ethics Committee of Kumamoto University Graduate School of Life Sciences.
2.3 Subjects
The respondents were 385 nurses and assistant nurses in six psychiatry hospitals that have gained research agreement in Prefecture A in Japan. They included psychiatric nurses in the nursing of patients with acute and chronic mental diseases, dementia, alcohol dependence, physical complications, and adolescent mental diseases. Responses were received from 347 psychiatric nurses in the first investigation (recovery rate 90.1%). Among the respondents, 302 people who gave their informed consent of the investigation were accepted as subjects for analysis (effective response rate 87.0%). Among the 302 people who gave informed consent for the first investigation, 181 people who had obtained agreement were accepted as subjects for analysis in the second investigation (effective response rate 59.9%).The firstand second data have been linked by subject’s date of birth.
2.4 Statistical analysis
The Mean and standard deviation (SD) was calculated for each variable. T-test of good-poor (GP) analysis was performed for the discriminative power. The exploratory analysis was performed for the extraction of factors. Cronbach’s alpha coefficients were calculated for the internal consistency as reliability of factors. Pearson’s correlation coefficients were calculated for an assumption off actor numbers, test-retest correlation as reliability, correlation between 11 items and convergent and predictive validity. The confirmatory factor analysis was performed for Good of Fit Index (GFI), Adjusted Goodness of Fit Index (AGFI), Comparative Fit Index (CFI) and Root Mean Square Error of Approximation (RMSEA) as Goodness-of-fit index for a factor stricture.
SPSS ver. 21.0 for Windows (IBM, New York, USA) was used for calculation of Mean ± standard deviation, the item analysis, and extraction of factors, calculation of Cronbach’s alpha and test-retest correlation coefficients as reliability, and calculation of convergent and predictive validity. Amos ver. 21.0 for Windows (IBM, New York, USA) was used for the calculation of factorial validity. In T-test of good-poor analysis in item analysis and Pearson’s correlation analysis of relevance between items, test-retest reliability and convergent and predictive validity, the significance level was set at P < .05.
3. Results
3.1 Subject characteristics
In characteristics of the 302 people who gave informed consent for the first investigation, the mean age was 42.47±11.19 (Mean ± SD). The gender was 96 males (31.8%), 197 females (65.2%) and 9 unanswered (3.0%). The job positions were 42 managers (head nurse or chief nurse) (13.9%), 233 non-managers (77.2%) and 27 unanswered (8.9%). The qualifications were 200 nurses (66.2%), 92 assistant nurses (30.5%) and 10 unanswered (3.3%). Experience in other departments was “Yes” by 201 people (66.6%), “No” by 91people (30.1%) and 10 unanswered (3.3%). The number of years of psychiatry department experience was 13.43±10.57 (Mean ± SD).
3.2 Item analysis
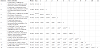
Each of the 10 item scores were divided into the upper 25% (high group: 76 subjects) and the lower 25% (low group: 76 subjects). Next, the discriminative power was analyzed by G-P Analysis. In addition, the Mean and SD were calculated, eliminating items with a ceiling effect and floor effect. Moreover, correlation coefficients between 11 items were calculated. In the results of the G-P Analysis for each item score, a significant difference (P< .01) between groups was confirmed in all 11 items (Table 1), and the discriminative power was demonstrated for each item. Then items did not have bias of all item distribution with no ceiling effect and floor effect in M±1SD. Significant correlation coefficients (P< .05) between 4 items related ‘Estimate of situation for psychiatric nursing’, 3 items related ‘Physical environment of the Psychiatric ward’ related 4 items of ‘Medical accident and unpredictable behaviors of psychiatric patients’ were confirmed. The number of missing values in each item was 0-6, which we judged to be small. Thus, the mean value was substituted for the missing values in the statistical analysis. In the second investigation, the number of missing values in each item was also 0-1, and the same analysis was done.
3.3 Exploratory factor analysis
The factor structure of the PNJSS (Supplemental version) was identified by factor analysis. An item (I feel a sense of burden from security management, such as locks and doors.) that showed less than .40 in one factor was deleted, and FA was repeatedly analyzed. In the process of conducting the FA, the Kaiser-Meyer-Olkin (KMO) measure of sampling adequacy was confirmed. The Maximum Likelihood Method was used in the extraction of factors, and promax rotation was conducted. Three factors were decided by the suggestion of table 1. Table 2 shows the results of FA. The KMO measure of sampling adequacy was .671, showing that it was acceptable to analyze by FA [22]. Three factors and 10 items were extracted. The first factor was named “Estimate of situation for psychiatric nursing (ESP)” to include 4 items related to the future of psychiatric patients. The second factor was named “Physical environment of the Psychiatric ward (PEP)” to include 3 items related to the physical environment of the Psychiatric ward. The third factor was named “Medical accident of psychiatric patients (MAP)” to include 3 items related to the medical accident and unexpected behaviors of patients.
3.4 Reliability of the PNJSS (Supplemental version)
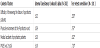
To consider the reliability of the PNJSS (Supplemental version), we performed a Cronbach’s alpha coefficient for each scale and subscale. Next, a correlation coefficient of each scale and subscale score between the first and second investigation was calculated to evaluate the test-retest reliability coefficient. Table 3 shows the results of the Cronbach’s alpha coefficient and the test-retest reliability coefficient. The Cronbach’s alpha coefficient was .619 for the scale and from .620 to .659 for each subscale. The test-retest reliability coefficient was from .520 to .797 (P< .01) for each subscale, a level from medium to strong. The test-retest reliability coefficient was .719 (P< .01) for the scale, a strong level.
3.5 Validity of the PNJSS (Supplemental version)
To examination the validity of the PNJSS (Supplemental version), the correlation coefficient with external variables was calculated for total scale and subscale score. In the convergent validity, the “job stressor” scale (JSS) of the “Brief Job Stress Questionnaire (BJSQ)” [23] and PNJSS were used as an external variable. To confirm the factorial validity, the compatibility of the factor model to the data was analyzed by CFA, and five goodness-of-fit indices were used (Goodness of Fit Index: GFI; Adjusted Goodness of Fit Index: AGFI; Comparative Fit Index: CFI; Root Mean Square Error of Approximation: RMSEA) [24]. Table 4 shows the results of the validity of the PNJSS (Supplemental version). In the results of convergent validity, the correlation coefficient was from -.068 to 0.563 between each scale and subscale score in the PNJSS (Supplemental version) and PNJSS and JSS, which was a level from weak to medium. In the results of predictive validity, the correlation coefficient was from .054 to .348 between each scale and subscale score in the PNJSS (Supplemental version) and SRS, which was a weak level. In the factorial validity, the result were χ2/df (57.844/32, P= .003) ratio =1.808, GFI= .965, AGFI = .940, CFI = .934, RMSEA = .052. The goodness-of-fit of the model was high. The result was shown as Figure 1.
4. Discussion
The aim of this study was to develop a PNJSS (Supplemental version) and test the reliability and validity of the scale. The following is a discussion of the results.
4.1 Examination of extracted factors
As we predicted, ESP factors included items related to the difficulty of foreseeing the lifestyles of psychiatric patients after hospital discharge and diagnosis in psychiatric nursing care. Japan has the longest mean duration of hospital stay for psychiatric inpatients in the world [12]. When the length of hospital stay becomes prolonged, patients become highly susceptible to “hospitalism” that includes weakened self-care ability [25]. Moreover, patients sometimes stop taking their medications after leaving the hospital [26], and patients that have been discharged from psychiatric wards have a high likelihood of being readmitted soon after [27]. These findings suggest that PNs have difficulty assessing hospital discharge for psychiatric patients or providing support that foresees their lifestyle after discharge. Psychiatric care is shifting from inpatient care at hospitals to community care [28,29]. The excessive amount of discharge support provided by PNs is related to the difficulty in providing such support, and may be one factor contributing to job stress.
As we had predicted, PEP factors included factors related to odors, cleanliness and feeling of oppression in the psychiatric ward. However, due to the structure of psychiatric wards, each door is often locked [15-17], and ventilation and temperature control are important. One study suggested that PNs feel that the ward environment is unsanitary and tend to sense odors more strongly when doors are locked, and that odors can be particularly stressful in their work [30]. A daily sense of odors in the psychiatric ward or a negative image of the ward may increase job stress for PNs.
As we predicted, MAP factors included factors related to patient suicide, self-harm, suspicious behaviors and medical accidents.
However, “I feel a sense of burden from security management, such as locks and doors” was removed from the factors. The association between stress of security management and of medical accidents was not strong. However, PNs does have stress related to medical accidents arising from sudden behavior by psychiatric patients. Individuals with mental disorders such as schizophrenia may have psychiatric symptoms that include hallucinations and delusions [31], and such psychiatric symptoms are often observed in psychiatric inpatients who commit suicide [32]. Moreover, suicide is sudden and unpredictable [33], and delusions of psychiatric patients are strongly connected to violence [18]. Suicide is a matter of the patient’s own livelihood, and violence and other impulsive behavior can harm others and cause medical accidents. In nursing care work, when PNs see psychiatric symptoms in patients on a daily basis, they may sense the danger of a medical accident, and this may cause job stress.
4.2 Examination of the reliability and validity of PNJSS (Supplemental version)
As shown in Table 1, three factors ESP, PEP and MAP were postulated from 11 items. Factor analysis confirmed the validity of 10 items for the three factors: four items for ESP, three for PEP and three for MAP (Table 2).
Regarding reliability of the PNJSS (Supplemental version), tests of internal consistency for the total scale and subscales gave Cronbach’s alpha coefficients of .619-.659 (Table 3). As they were all over .60, they were all deemed to be at an allowable level [34]. Furthermore, a test of test-retest reliability of the total scale and subscales of the PNJSS (Supplemental version) gave correlation coefficients of .520- .797, with strong correlation coefficients of significance within the 1% level. We therefore deemed the total scale and subscales of the PNJSS (Supplemental version) to have strong test-retest reliability.
Regarding the validity of the PNJSS (Supplemental version), tests of convergent validity confirmed positive correlations within a significance of p<.05-.01 for many of the associations among the total scale and subscales of the PNJSS (Supplemental version), PNJSS and JSS (Table 4). We therefore deemed the PNJSS (Supplemental version) to be capable of assessing job stressors. Tests of predictive validity also confirmed positive correlations within a significance of p<.05- .01 for almost all of the associations between the total scale and subscales of the PNJSS (Supplemental version) and the SRS (table 4). We therefore deemed the PNJSS (Supplemental version) to be capable of predicting stress reactions. In addition, tests of factorial validity by CFA gave goodness-of-fit values for the model of χ2/df (57.844/32, p<0.01) ratio =1.808, Good of Fit Index (GFI) = .965, Adjusted Goodness of Fit Index (AGFI) = .940, (Comparative Fit Index (CFI) = .934 and Root Mean Square Error of Approximation (RMSEA) = .052(Figure 1). This values are stronger than validity criteria (χ2/df ratio<2.0 [35], GFI> .90, AGFI> .85, CFI> .95 and RMSEA<0.08 [36]. We therefore deemed the PNJSS (Supplemental version) structure of 10 items in three factor categories to be valid.
5. Limitations of the Study
As this study only investigated PNs in Prefecture A, we cannot rule out the possibility of a selection bias due to distinctive characteristics of that prefecture’s residents. Further studies on subjects from other prefectures as well are needed to minimize this selection bias.
6. Conclusion
We extracted 10 items in three factor categories (four items for ESP, three for PEP and three for MAP) that may be considered job stressors in PNs and confirmed adequate reliability and validity. The PNJSS (Supplemental version) may thus be considered a useful new tool for assessing job stressors unique to PNs that cannot be assessed with the original PNJSS. While the PNJSS has been confirmed to have adequate reliability and validity, use in conjunction with the Supplemental version may enable a more detailed assessment of job stressors in PNs.
Competing Interests
The author has no conflict of interest directly relevant to the content of this article.
Author Contributions
Hironori Yada, Hiroshi Abe, Hisamitsu Omori, Yasushi Ishida, and Takahiko Katoh designed the research and wrote the paper; Hironori Yada performed the research; Hironori Yada analysed the data.
Acknowledgments
We thank several medical doctors and psychologist (Hiroshi Taniguchi, Hiroyuki Hashiguchi, Hisae Matsuo, Izumi Wakimoto, Jyungo Nakamura, Ryoei Miyoshi, Shigeki Kurayama, Syouhei Makita, Yoshio Mitsuyama, and YoukoTsuyama) and the nurses in the psychiatric departments of the study hospitals for their cooperation in this study.